Based on current studies and anecdotal evidence, several urologists feel it’s relatively safe to administer Testosterone Replacement Therapy (TRT) for men with prostate cancer who are on active surveillance or those who have been treated with prostatectomy or cryosurgery.
Based on current studies and anecdotal evidence, several urologists feel it’s relatively safe to administer Testosterone Replacement Therapy (TRT) for men with prostate cancer who are on active surveillance or those who have been treated with prostatectomy or cryosurgery.
However, they emphasize that it is critical that these men should be closely monitored.
In the past, TRT was not considered for men suffering from prostate cancer. But, based on new research, times have changed, and TRT is often prescribed for prostate cancer patients, according to Wayne J.G. Hellstrom, MD, professor of urology and chief of andrology at Tulane University School of Medicine in New Orleans, Louisiana.
Orleans, Louisiana.
“About 20 years ago, when I gave a course at the American Urological Association [AUA] and would ask if anybody in the audience would give testosterone to a man who had prostate cancer, 3 of maybe 300 to 400 urologists would put up their hands. Now, probably 75% to 80% of urologists will give testosterone to men in these circumstances,” he stated. Until recently, he added, urologists were reluctant to give testosterone to men with prostate cancer for fear of “fueling the fire.”
This fear was due to a study in the 1940s by Dr. Charles Huggins that found a link between androgenetic hormones and prostate cancer, according to Dr. Arthur L. Burnett II, MD, professor of urology at Johns Hopkins University in Baltimore, Maryland. Recent guidelines, however, are varied and do not always confirm the findings of Dr. Huggins.
The latest guidelines
The authors of an editorial comment published earlier this year in the International Brazilian Journal of Urology found: “Last guidelines’ revisions show some changes on CaP [prostate cancer] as a definitive contraindication for TRT [testosterone replacement therapy]. The Endocrine Society has the strictest guidelines, advising against T in patients with an unevaluated prostate nodule, PSA >4ng/mL, or PSA >3ng/mL in high-risk patients (i.e., African Americans or a first-degree relative with CaP). Only the AUA and ISSM [International Society for Sexual Medicine] recommend offering T on a case-by-case basis for all patients with CaP. Patients treated for localized CaP with no evidence of active disease (measurable PSA, abnormal digital rectal examination findings, evidence of bone or visceral metastases) are candidates for replacement under the Canadian Medical Association Journal, European Association of Urology (EUA), and British Society for Sexual Medicine guidelines (BSSM).”
"There are no randomized placebo-controlled trials giving men testosterone therapy after prostate cancer treatments. However, initial studies have not demonstrated any increased risk of biochemical recurrence,” according to Mohit Khera, MD, professor of urology at Baylor College of Medicine in Houston, Texas. He added that the AUA released its guidelines in 2018, recommending clinicians should inform patients of the absence of evidence linking testosterone therapy to the development of prostate cancer,
“However, the guidelines go on to state that patients with testosterone deficiency and a history of prostate cancer should be informed that there is inadequate evidence to quantify the risk-benefit ratio of testosterone therapy,” he said.
“This was based on expert opinion. There are no randomized placebo-controlled trials giving men testosterone therapy after prostate cancer treatments. However, initial studies have not demonstrated any increased risk of biochemical recurrence.”
Every patient is unique.
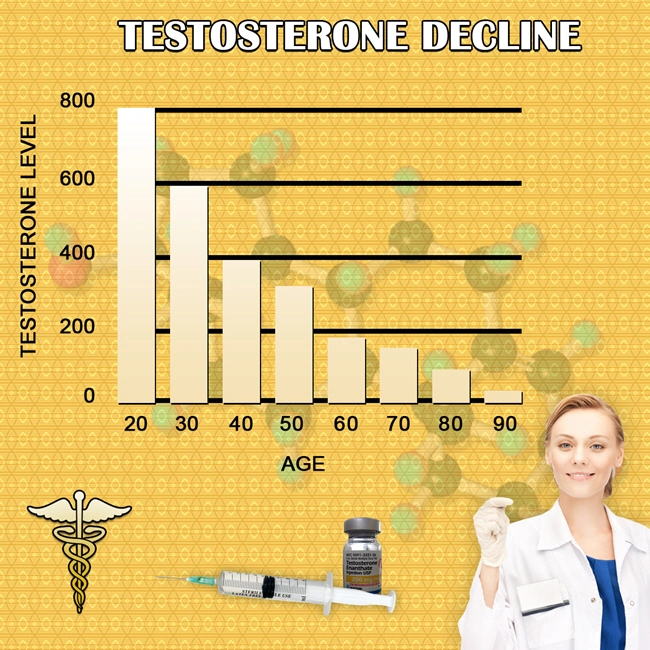
Men with symptoms of low testosterone (aka “Low-T”) can experience relief, including increased muscle mass, a boost in mood, less brain fog, and an awakened libido from TRT. “A significant number of men as they age are more likely to have prostate cancer, but they’re also more likely to have symptomatic hypogonadism, and treatment may be warranted for these guys,” noted Hellstrom.
 According to Khera, testosterone might play a vital role in prostate cancer patients' health and quality of life. “Specifically for men with a history of prostate cancer, testosterone therapy can improve recovery of erectile function following…treatment. Testosterone plays a key role in overall erectile function.”
According to Khera, testosterone might play a vital role in prostate cancer patients' health and quality of life. “Specifically for men with a history of prostate cancer, testosterone therapy can improve recovery of erectile function following…treatment. Testosterone plays a key role in overall erectile function.”
Although every case is unique, Hellstrom said he does not worry about starting or continuing TRT in certain patients. “As far as patients who have localized prostate cancer on surveillance and those men who have had local therapy, which may be radical prostatectomy, radiation, or cryotherapy, there is really no good evidence that men are worse off if they are hypogonadal and treated appropriately,” he pointed out.
“It’s important that those men who are treated recognize that they need to be followed closely, which involves testosterone [level monitoring], PSA [prostate-specific antigen], and digital rectal exams every 3 to 6 months during treatment.”
Dr. Burnett II said, “In a man who gets the diagnosis and has high-grade disease, the PSA [level] is rapidly going up, and on top of that, he says he gets a so-so benefit from the testosterone, you’d say then let’s withdraw the testosterone.”
For Burnett, things get disquieting as prostate cancer progresses or there is metastatic disease: “If the PSA [level] is rapidly increasing, you know that prostate cancer is increasing in the body, and that would increase my hesitancy about testosterone replacement.”
Not everyone agrees. Treating men with metastatic prostate cancer is still highly controversial due to the fear that TRT will increase the chance the cancer will grow, Hellstrom said.
However, he added that this is being tested by investigators studying intermittent high-dose androgen therapy in men with metastatic prostate cancer and seeing that “in a significant number of these men, the actual prostate cancer and the PSA levels regress.”
Should urologists stop TRT when men are first diagnosed with prostate cancer? Not necessarily, but for Khera, there is an exception, and that is “the patient who is going on to receive radiation therapy and will require androgen deprivation therapy [ADT]. In these patients, we stop testosterone in preparation to start ADT.”
In most cases of early disease, these physicians think it’s safe to keep men with no evidence of metastases on testosterone. “I would keep him on it with the understanding that he has close follow-up,” Hellstrom said.
According to Khera, urologists should decide to continue therapy on a case-by-case basis, depending on the Gleason score, tumor grade and stage, and anxiety and tolerance levels.
“If it’s pretty low-threat prostate cancer and a man says I’d rather jump off a cliff than stop my testosterone, then I might say, ‘I want you to hear all the risks, but I can’t oppose you using it,’” Burnett added, noting that in every case, including new diagnoses, it’s crucial to consider the benefit a man gets from taking testosterone.
“In a man who gets the diagnosis and has high-grade disease, the PSA [level] is rapidly going up, and on top of that, he says he gets a so-so benefit from the  testosterone, you’d say then let’s withdraw the testosterone.”
testosterone, you’d say then let’s withdraw the testosterone.”
“We are recognizing that testosterone therapy can be beneficial when correctly administered in prostate cancer patients,” Burnett said. “However, a lot of this is anecdotal, and some is a bit of the Wild West regarding the safety of who can and cannot be treated with it, considering where the literature is right now,”
The good news is that investigators are starting to conduct randomized controlled trials, including researchers from Johns Hopkins and Brigham and Women’s Hospital, in Boston, Massachusetts, to determine the potential benefits and risks of TRT in men treated for prostate cancer.
“We’re trying to make a statement that may afford the urologists out there the necessary literature support, so if they put somebody on therapy, they can really counsel them,” Burnett said.
Reference
Javaroni V. Editorial comment: testosterone replacement therapy (TRT) and prostate cancer: an updated systematic review with a focus on previous or active localized prostate cancer. Int Braz J Urol. 2022;48(1):188-195. doi:10.1590/S1677-5538.IBJU.2022.01.08
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Injectable HGH Prescriptions: Blood Testing Centers in Philadelphia, Pennsylvania [Last Updated On: August 27th, 2025] [Originally Added On: March 3rd, 2019]
- Nutropin Hgh: Hgh Hormone Product [Last Updated On: December 21st, 2024] [Originally Added On: March 10th, 2020]
- Hgh Replacement [Last Updated On: December 21st, 2024] [Originally Added On: March 14th, 2020]
- Hgh Therapy [Last Updated On: December 22nd, 2024] [Originally Added On: March 15th, 2020]
- Anti-ageing Clinics Distribute Human Growth Hormone [Last Updated On: December 25th, 2024] [Originally Added On: March 16th, 2020]
- Hgh In Forefront To Remain Young [Last Updated On: November 25th, 2024] [Originally Added On: March 18th, 2020]
- Benefits Of Hgh: Thierry Hertoghe [Last Updated On: December 23rd, 2024] [Originally Added On: April 23rd, 2020]
- Getting Started With An Hgh Program [Last Updated On: December 24th, 2024] [Originally Added On: April 25th, 2020]
- Hgh Releasers [Last Updated On: December 25th, 2024] [Originally Added On: April 26th, 2020]
- What dietary considerations should I make while on HRT, hormone replacement therapy? [Last Updated On: December 20th, 2024] [Originally Added On: May 1st, 2020]
- Hgh Dosage [Last Updated On: March 3rd, 2025] [Originally Added On: May 5th, 2020]
- Hgh Deficiency [Last Updated On: December 23rd, 2024] [Originally Added On: May 6th, 2020]
- Hgh Products Genotropin Humantrope Nutropin Saizen Serostim Omnitrope [Last Updated On: November 25th, 2024] [Originally Added On: May 8th, 2020]
- What Is Injectable Hgh Human Growth Hormone? [Last Updated On: December 22nd, 2024] [Originally Added On: May 9th, 2020]
- Introduction To Human Growth Hormone HGH [Last Updated On: December 24th, 2024] [Originally Added On: May 10th, 2020]
- Omnitrope Injections for the Treatment of HGH Deficiency [Last Updated On: June 15th, 2025] [Originally Added On: May 6th, 2021]
- Sleep To Amplify Human Growth Hormone Levels [Last Updated On: June 14th, 2025] [Originally Added On: May 27th, 2021]
- Buying Hgh Hormone Human Growth Hormone [Last Updated On: August 20th, 2025] [Originally Added On: February 22nd, 2022]
- Hgh For Menopause [Last Updated On: October 28th, 2025] [Originally Added On: February 23rd, 2022]
- Your HGH Levels [Last Updated On: October 5th, 2025] [Originally Added On: February 24th, 2022]
- Related Glossary of Terms [Last Updated On: October 14th, 2024] [Originally Added On: February 25th, 2022]
- Hgh Facts - Information About Growth Hormone [Last Updated On: August 21st, 2025] [Originally Added On: February 26th, 2022]
- Hgh Sports And Baseball [Last Updated On: August 22nd, 2025] [Originally Added On: February 27th, 2022]
- Us Olympic Committee And Talk Of Hgh [Last Updated On: October 30th, 2025] [Originally Added On: February 28th, 2022]
- Braves' Schafer Talks About His Suspension Over Hgh [Last Updated On: August 23rd, 2025] [Originally Added On: March 1st, 2022]
- Hgh Scams: Different Hgh Scams And Things To Watch For Online [Last Updated On: August 27th, 2025] [Originally Added On: March 2nd, 2022]
- Nordiflex HGH Injection Device Information [Last Updated On: October 31st, 2025] [Originally Added On: March 3rd, 2022]
- Genotropin Hgh Detailed Description [Last Updated On: October 15th, 2024] [Originally Added On: March 4th, 2022]
- Saizen Hgh Detailed Description [Last Updated On: October 17th, 2024] [Originally Added On: March 6th, 2022]
- Genotropin HGH: Human Growth Hormone Product [Last Updated On: August 24th, 2025] [Originally Added On: March 6th, 2022]
- Omnitrope Hgh: Human Growth Hormone Product Called Omnitrope. [Last Updated On: October 5th, 2024] [Originally Added On: March 7th, 2022]
- Nutropin Hgh Detailed Description [Last Updated On: November 3rd, 2025] [Originally Added On: March 8th, 2022]
- Saizen Hgh: Injectable Hgh Product [Last Updated On: August 25th, 2025] [Originally Added On: March 9th, 2022]
- Hgh Product Serostim [Last Updated On: August 26th, 2025] [Originally Added On: March 11th, 2022]
- HGH Scams (HGH Supplements) [Last Updated On: November 12th, 2024] [Originally Added On: March 20th, 2022]
- Side Effects Of HGH [Last Updated On: September 3rd, 2025] [Originally Added On: March 21st, 2022]
- Testimonial: Walter’s HGH Story [Last Updated On: September 28th, 2025] [Originally Added On: June 4th, 2022]
- HGH Is the “God Particle” [Last Updated On: September 17th, 2025] [Originally Added On: July 26th, 2022]
- Low testosterone in men might increase the risk of severe COVID [Last Updated On: October 21st, 2025] [Originally Added On: September 6th, 2022]
- Can I Reverse the Aging Process with HGH? [Last Updated On: September 19th, 2025] [Originally Added On: September 21st, 2022]
- A new study confirms: Testosterone Replacement Therapy is safe! [Last Updated On: October 4th, 2025] [Originally Added On: October 2nd, 2022]
- HGH Therapy – How Can I Know Who Is Legitimate? [Last Updated On: June 7th, 2025] [Originally Added On: January 10th, 2023]
- Nine Hormones that Can Impact Your Weight and How to Promote Hormone Balance [Last Updated On: June 6th, 2025] [Originally Added On: January 26th, 2023]
- Get Tested for Hormone Levels, even if You Have No Symptoms [Last Updated On: September 29th, 2025] [Originally Added On: March 17th, 2023]
- Can Head Injuries Cause HGH Deficiency? [Last Updated On: September 26th, 2025] [Originally Added On: May 17th, 2023]
- Mountain Biker Thought his Life Was Over [Last Updated On: September 15th, 2025] [Originally Added On: May 25th, 2023]
- Do HGH Booster Supplements Work Faster Than Prescriptions? [Last Updated On: October 1st, 2025] [Originally Added On: June 3rd, 2023]
- HGH and It’s Effects on Other Hormones [Last Updated On: October 26th, 2024] [Originally Added On: June 10th, 2023]
- Maintaining a Proper Medication Schedule [Last Updated On: November 24th, 2024] [Originally Added On: August 23rd, 2023]
- What is the History of the Discovery of HGH? [Last Updated On: October 21st, 2024] [Originally Added On: September 17th, 2023]
- Don’t Let Fear Stop You From Fixing Your Hormones [Last Updated On: October 22nd, 2024] [Originally Added On: September 22nd, 2023]
- Understanding HGH Dosage [Last Updated On: February 26th, 2025] [Originally Added On: February 26th, 2025]