The Facts You Need to Know About Testosterone
Video Link: https://vimeo.com/260619631
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/260619696
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/260619748
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/260621533
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Q: What is Testosterone?
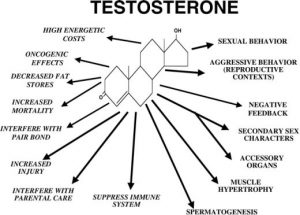
A: Testosterone is a hormone, a chemical messenger – it is the sex hormone that is responsible for making males male, although women also have the hormone in small amounts. Also known as an androgen, Testosterone is produced mostly by the testes/testicles. The Leydig cells,  present in certain parts of the testis, produce Testosterone.
present in certain parts of the testis, produce Testosterone.
Men are infertile without Testosterone – during the process of spermatogenesis (development of mature sperm), germ cells are unable to progress beyond meiosis (reproductive cell division) in the absence of Testosterone.
Q: Why should I consider Testosterone Replacement Therapy (TRT)?
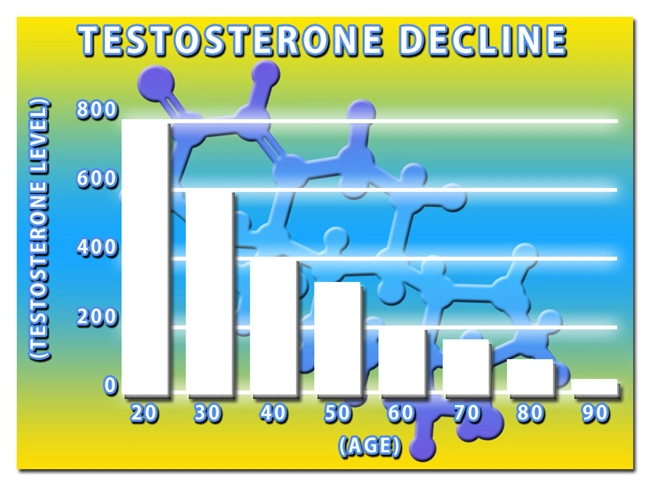
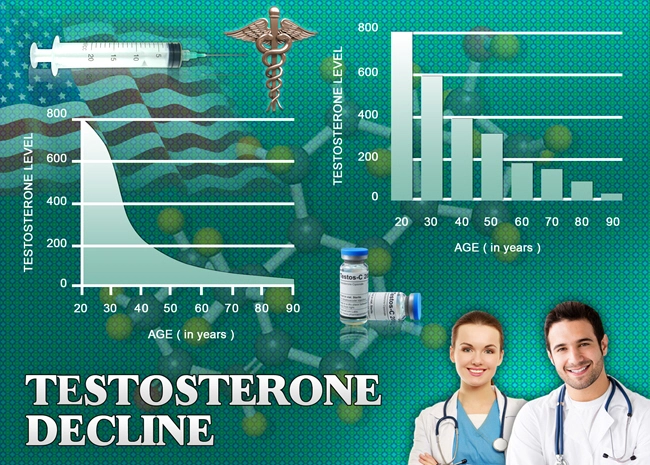
A: A man's testosterone levels begin to drop around age 30 at a rate of approximately 10% per decade. This slide introduces a broad range of health problems: lowered libido, erectile dysfunction, increasing joint aches, and pain, weakened, soft muscle tone and loss of strength, increased layers of ugly, disease-producing fat, mental fog and an inability to concentrate, chronic tiredness with the lack of energy, and depression.
While many medical professionals continue to state that “this is just a natural part of the aging process” and proclaim that nothing can be done about it, more and more men and their physicians are seeing the results of Testosterone Replacement Therapy and are giving it a try. The results? A stop to the health problems listed above, or at least slowing them down to a crawl.
Q: Testosterone Replacement Therapy is controversial. Could you explain why?
A: The crux of the medical ethics issue is this: are people taking Testosterone to cure a disease, or are they using it to transcend the limitations usually imposed on an aging human body?
What the Medical Professionals Say
Dr. John Hoberman, the author of Testosterone Dreams, thinks that’s a question many more of us will be asking in the coming years. “The 21st century is going to be a testing ground for what the human race decides to do regarding its self-transformation,” he said. In fact, as the growth of Testosterone usage proves, we’ve already begun.
Testosterone has shown itself to be a miracle drug for many, and it can be a life-changer. Users, who had been evaluated and have low levels of Testosterone report increased energy, more muscle mass, decreased body fat, greater sex drive, and a general sense of well-being. Also, the number of users is growing.
Here's a look at a physician who advocates TRT: At 56, Dr. Paul Campion is in better shape than he was in his 30s. He proudly shows pictures showing the belly he carried three years ago before he began taking Testosterone supplements.
belly he carried three years ago before he began taking Testosterone supplements.
That was then; this is now. His abdominal's have shed their flab, and he is now “ripped.”
Before starting TRT, Campion was an eye doctor, struggling to stay in shape, like so many aging men. “I was just at the gym watching the 30-year-olds at the pull-up bar building muscles in three weeks. And I’m at the pull-up bar, and nothing’s happening,” he recalls. “I’m not feeling good. I’m sleepy all the time. All I want to do is sit down and eat potato chips and watch TV. Something’s not right.”
So he found Cenegenics, a medical start-up that trains physicians to run their own “age management” practices. They revamped his diet, put him on a new workout routine, and started giving him Testosterone. Within six months, his body fat plunged to nine percent. “That’s pretty hard to maintain — I’m closer to 12 per cent now,” he brags. After his success, Cenegenics asked if he’d like to take their training course.
He agreed and quickly switched specialties and business models. He became a Testosterone doctor. Clinics like his "don’t work like most doctors’ offices do," where they are limited by what insurance companies will pay. He runs an all-cash business.
The initial session costs $5,000, and the monthly charges are over $1,000. Clients get their blood work done every three months so that Campion can keep tabs on how their “hormonal balancing” is going.
Most patients stay on Testosterone permanently, as Campion has. “I will take testosterone for the rest of my life,” he says. Testosterone is not just any drug. It is as close to a direct anti-aging medication as science has yet produced.
It can be manufactured cheaply in large quantities, and the risks seem manageable for most people. Users report increased energy, more muscle mass, decreased body fat, greater sex drive, and a general sense of well-being. In sum, it’s one of the most transformative substances a human can take.
A Powerful and Efficient Drug
“Testosterone is ridiculously powerful,” Campion says. “I can tell you from experience, the feeling of well-being, of focus, and of masculine energy are massively increased. It’s like you’re back to being 35.” That power — a long with a heavy dose of pharma company marketing — is why millions of American men are obtaining Testosterone from doctors in various forms.
According to a study by University of Texas epidemiologist Jacques Baillargeon, nearly four per cent of men in their 60s are taking Testosterone. The number of men between 40 and 64 went up 77 per cent from 2010 to 2013 to 1.5 million men. Abbvie, the maker of a popular Testosterone gel, is raking in more than a billion dollars a year from the sale of AndroGel.
In 2013, 14,000 kilograms of Testosterone were sold in the United States. That might not sound like much, but a typical adult male has just 0.000000035 kilograms of Testosterone floating around in his blood. There are tons of extra Testosterone in the hormonal composition of the country — and it only accounts  for the legal sales.
for the legal sales.
The rising popularity of Testosterone has opened up whole new business models for entrepreneurial doctors. Chains of shops that provide the hormone have exploded all over the United States.
How many millions of more men might be willing to try Testosterone if it was easy to acquire, and a clinic happened to implant itself in an adjacent office building or a local strip mall, next to an abandoned video store and the Starbucks?
We don’t need to look ahead at human genetic engineering, brain implants, or crazy designer drugs to see the real future of our relationship with our bodies.
The rise of Testosterone use isn’t a drill for future body-hacking — it is body-hacking playing out right now across the American heartland, with a substance that was first synthesized in 1935. And in the coming years, the battles over Testosterone use are going to be repeated for future drugs that give people — anyone with money, at least — the power to transform the body beyond its innate abilities and configurations.
Campion insists that his Testosterone clinic is meant to promote well-being, not to cure disease, even though he uses the tools of medicine. “Our philosophy is to stay out of medical buildings, even though we are medical doctors because we don’t want to be sick-oriented,” Campion says. “I don’t prescribe any ‘sick’ medicines. I prescribe hormones and supplements.”
There’s another complex set of ideas at play, too. The Testosterone story is easy to tell in a way that focuses on older, wealthy men. They’re the ones who want to recapture the vitality of their fading youth. This tale is yet another version of the age-old story about power and staying youthful and vibrant, regardless of risks or costs.
Aging: Just Like Any Other Disease
These are not merely abstract, philosophical questions. What’s at stake is not only the ethical future of the medical community but the boundaries of human life. Here’s how the classical medical model is supposed to work. A man goes to a doctor. He says he has X and Y problems, may be low energy and sex drive, plus a gut. The doctor runs some blood tests, finds the man has low testosterone levels, and diagnoses his condition as hypogonadism. Testosterone is prescribed to treat that condition.
That’s the clinical guideline provided by The Endocrine Society, the nation’s foremost professional association of hormone-focused doctors, at least. Harvard urologist Abraham Morgentaler has been an outspoken proponent of Testosterone Replacement Therapy for years. He’s written several books on the topic, including the best-selling Testosterone for Life. Morgentaler’s view is simple: Testosterone is like any other drug.
Hypogonadism, in which free Testosterone levels fall below a rather ill-defined threshold, is like any other disease. “Men have symptoms that are related or possibly related to a deficiency of a hormone, and if the symptoms are bothersome, then the men will undergo a trial of treatment, and it is often but not always successful,” Morgentaler said. “This is what we do in medicine. There is nothing that’s different.”
But is it really that easy? Is there nothing different? Testosterone falls as men get older, so isn’t giving them Testosterone an attempt to  reverse aging? Morgentaler answers as if he’d heard it countless times. “The drop in testosterone is natural because it occurs so commonly and therefore it is a natural part of aging.
reverse aging? Morgentaler answers as if he’d heard it countless times. “The drop in testosterone is natural because it occurs so commonly and therefore it is a natural part of aging.
So why should we treat something that is healthy aging?” he said. “And the response is that almost everything we treat in medicine is age-related. Aging is related to bad eyesight, bad hearing, bad joints, bad hearts, bad blood vessels, and cancer.
We treat all of these without trying to minimize or diminish them that they are age-related. And they are, no less than the deficiency of testosterone.” One might concede the point: prevalence and age-linkage do not make Testosterone different. What makes Testosterone different is Testosterone itself. Testosterone isn’t like giving someone a hearing aid, or a new pair of glasses.
Testosterone is a vital part of the body’s essential communication and regulatory systems. Hormones partially control how the genes coded into a genome get used. Change someone’s Testosterone level, and you change the whole organism. In 2002, The New Yorker ran a profile of Morgentaler.
In it, Morgentaler concludes two visits with patients using roughly the same line, “If I had a magic wand and I could do anything for you, what would it be?” The patients name different things — “the energy thing” or “the problem with orgasm” — but the solution is the same, Testosterone. Testosterone can be a magic man wand.
Bodybuilders of the Arnold Schwarzenegger era and baseball players of the Barry Bonds era have given us a series of caricatures of what Testosterone can do to a body. But Morgentaler says steroid users aim for Testosterone levels 50 to 100 times normal Testosterone levels. So, that’s not what happens when you undergo Testosterone Replacement Therapy.
And yet, the effects of Testosterone on the body are still fascinatingly powerful at lower levels. As these stories show, it is no longer the case that one must be diagnosed with a disease to get Testosterone from a doctor. Individual doctors are slowly pushing the boundaries of traditional medical practice so they can give their patients what they want.
They're trying to resolve what our society has not been able to decide: should a more-or-less healthy person who merely wants to change his or her body with a drug be allowed to do that? After all, the doctors are only helping their patients do what contemporary society wants them to do.
“No matter what you consider a disease or condition, the fact remains that by the time you reach 40-45, virtually every man has lowering Testosterone. That’s a natural state of being as you slowly poop out. But we’re around a lot longer than that,” said Campion. “I say, why not stay in the optimal shape that you have? Hormones, we know, keep you useful. So why the heck aren’t we using them?”
Dr. Hoberman argues in Testosterone Dreams that the fact that Testosterone helps people meet societal aspirations is why it’s so difficult to regulate.  Taking Testosterone isn’t making you escape reality; it’s helping you stay energetic and healthy.
Taking Testosterone isn’t making you escape reality; it’s helping you stay energetic and healthy.
“Once upon a time, respectable society feared contamination by illegal and disreputable drugs that were consumed by social deviants,” he writes.
“Now regulators are concerned about a growing demand for legal drugs that serve socially sanctioned goals such as productivity, physical attractiveness, and sexual viability.
The ‘threat’ posed by such drugs originates in the very system of values that authorizes their use, and it is a paradox that has put regulators in an untenable position.”
A New Medical Model
A new medical model has emerged that Hoberman calls “client-centered libertarian medicine.” Doctors become service providers, and the people formerly known as patients are their clients. The entrepreneurial medical model around Testosterone pays little attention to previous cultural norms that previously constrained prescribing it.
Can anyone find a doctor to put them on hormones with little or no testing evidence? The answer is yes. Part of the problem is that it is no longer possible to rely on American doctors generically speaking to practice responsible medicine with hormones.
But many disagree...and the debate rages on and on. This emergent industry is not primarily composed of high-end, coastal practices like Campions.
"Low-T" business startups are sprouting up across the country, most run by entrepreneurial doctors who did not specialize in endocrinology, urology, or any related subfield. At last count, two of the largest chains alone — Body Logic MD and Ageless Men’s Health — have added more than 150 locations since the late 2000s. (And that’s to say nothing of the small chains like Epoch Health, or the thousands of general “anti-aging” clinics that deploy a full array of pharmacological options.)
 “That’s a whole industry that is, to me, an opaque phenomenon right now,” Baillargeon — the University of Texas epidemiologist — stated. “I haven’t seen any real rigorous scientific studies of the low-T private clinics. It’d be interesting to know how many young guys with normal testosterone levels get treatment from those types of places.”
“That’s a whole industry that is, to me, an opaque phenomenon right now,” Baillargeon — the University of Texas epidemiologist — stated. “I haven’t seen any real rigorous scientific studies of the low-T private clinics. It’d be interesting to know how many young guys with normal testosterone levels get treatment from those types of places.”
The darkest dens of the Testosterone industry can be found on the Internet, where websites broker connections between men seeking Testosterone therapy and networks of doctors who have an affiliation with the web service. One, Andrologix, claims thousands of patients.
The gray-market, mostly-unregulated nature of these services has led to some investigations, including one by the Food and Drug Administration (FDA), which found that fully half of the men taking Testosterone hadn’t been diagnosed with the disease hypogonadism.
A full quarter of them did not even have blood work done before they were given hormones. Many medical professionals would be alarmed at these statistics, but may be they are overreacting. Alcohol is legal, as is smoking, overeating, being a couch potato, and sky-diving. What if a nation full of strip-mall, cash-only Testosterone clinics is added to that mix?
A New Age of Human Enhancement
That’s certainly the position of Julian Savulescu, an Oxford philosopher and somewhat notorious proponent of human enhancement. “I think aging is the greatest evil that we face. Two-thirds of people die through aging. I’m all for turning off the effects of aging,” Savulescu told me. “And I’m totally behind the idea of human enhancement.” Savulescu has reached his position through what he calls a common-sense approach to TRT.
If there are large benefits to be had by enhancing human beings with relatively minimal risks, then, he argued, we should do it. “It’s just an outdated way of thinking that says, ‘The only thing that matters is a disease,’” and not more general health as expressed through one’s biological body. “People want to chop off healthy limbs, or a healthy penis, or they don’t want to get old, or they want to have sex at the age of 85.
There is nothing unreasonable about those things,” he said. “It doesn’t have to be 100 per cent safe. Life is never 100 per cent safe.” And yet, when it comes  to Testosterone, Savulescu, who is 51, doesn’t think that the messy American compromise of entrepreneurial doctors dosing out tons of Testosterone prescriptions is the right approach.
to Testosterone, Savulescu, who is 51, doesn’t think that the messy American compromise of entrepreneurial doctors dosing out tons of Testosterone prescriptions is the right approach.
Men can’t be expected to assess the medical risks of taking Testosterone adequately, he said. “And I wouldn’t want some guy who opened up a clinic to make money selling testosterone telling me what the data was,” he said.
Worse, he said, the look-the-other-way American compromise to human enhancement through Testosterone means that data is not being captured about any of the healthy people who are taking Testosterone and other enhancers.
“There are all these people on modafinil [a cognitive enhancer], testosterone, growth hormone, and we have no idea what’s happening to them. That data is available,” he noted. “This idea that the only way that we proceed is through a randomized, double-blind, controlled trial for some disease — it’s deeply out of kilter with modern life. And we ought to be thinking about experiments in a much wider range of instances. We don’t have to put everyone in a laboratory, but we should be getting data.”
The Food and Drug Administration (FDA) Weighs In
Of course, the FDA is a monstrous bureaucracy that is designed to do those randomized, double-blind, controlled trials, and that's all. Its other job is to make sure that drugs are only used to treat diseases. So, this brings up the question: is a new regulatory agency needed that could handle other types of treatments?
Yes, indeed, Savulescu said. “I think it should be the Human Well-Being Regulatory Authority,” he said. “And it should be about looking at biologics and the sorts of interventions that the FDA looks at, just not regarding disease but human well-being.”
Such a hypothetical agency could ensure the safety of drugs and drug prescribers without constraining precisely what they would be used for. And it would gather data on the outcomes of the pharmaceutical regimens that people chose to follow.
It goes without saying that this would be a radical, radical departure from the current way of regulating drugs in America. Manhood is the central preoccupation of the sales pitch for Testosterone.
One typical Androgel commercial takes place on a construction site in which men construct the Androgel  brand name at building-scale. Androgel’s website tells visitors, “You are a man. You want facts. You get down to business. You might have low testosterone. You don’t like wasting time. You’re visiting this site for a reason.”
brand name at building-scale. Androgel’s website tells visitors, “You are a man. You want facts. You get down to business. You might have low testosterone. You don’t like wasting time. You’re visiting this site for a reason.”
The demand for Testosterone, then, is not solely determined by the pharmaceutical companies' advertising. The way our society requires men to feel and act creates the social context for the explosion of “low T” and the emotional resonance of Testosterone marketing.
Testosterone Use Grows
So, you want to perform manhood more efficiently? Take some Testosterone. The sheer fact that properties of “manhood” can be conferred by injection should destabilize our notion of how fixed in our bodies and identities we are. Toby Beauchamp, a University of Illinois gender studies professor, argued in a 2012 journal article about Testosterone regulation that the demand for Testosterone “overtly demonstrate[s] the fluidity of sex and gender categories.”
And yet, those same vials are being used by men to adhere more closely to the rigid gender norms to which most men in the country aspire. The demand for Testosterone didn't come from anywhere; it came from men wanting to be seen as manly.
And if some country did create a Human Well-Being Regulatory Authority, understanding why people would want to take a drug like Testosterone would be as important as assuring its safety. In fact, as the growth of Testosterone usage proves, we’ve already begun.
Q: What are normal testosterone levels?
A: An individual's Testosterone levels are determined through a blood test called a "serum total testosterone test." Testosterone exists in your blood stream in two forms -- "bound" Testosterone and "free" Testosterone.
The majority of bound Testosterone in the body is chemically bound to a protein called "sex hormone-binding globulin" (SHBG). The remaining bound Testosterone in the system is mostly bound to albumin, another protein. Free Testosterone is not chemically attached to any proteins and is considered the "active" form of Testosterone, as it is readily available to bind to androgen receptor sites on cells.
A serum total testosterone test measures the total of bound and free Testosterone in the system. What is considered an average test level of combined bound  and free Testosterone in male bodies can range anywhere from 300-1,100 ng/dl (nanograms per deciliter)? These levels will vary with age and individual factors.
and free Testosterone in male bodies can range anywhere from 300-1,100 ng/dl (nanograms per deciliter)? These levels will vary with age and individual factors.
Additionally, it is useful to individually measure the standard of free Testosterone in the system, as this may be a better indication of how hormone therapy is progressing.
Levels of free Testosterone can range between 0.3%-5% of the total Testosterone count, with about 2% considered an optimal level. Make sure your doctor checks for both total and free levels of testosterone in your system.
Remember, since everyone has different sensitivities to androgens, Testosterone levels themselves will not necessarily indicate results regarding masculinization. The levels are merely a guideline by which you and your doctor can begin to measure progress.
Your results and your dosing should be guided by your overall health (especially the health of your heart and liver) and how your body and moods react to different dosages. Testosterone therapy is not a cookie-cutter, one-size-fits-all approach. Make sure you monitor your health and feelings closely and remember that even a small adjustment in dosage (either increase or decrease) can make a big difference.
Stay Safe
Q: Are there any risks involved with Testosterone Replacement Therapy?
A: Yes. Known side effects of TRT include acne/oily skin, mild fluid retention, stimulation of prostate tissue, with perhaps some increased urination symptoms such as a decreased stream or frequency, breast enlargement, worsening of sleep apnea (a sleep disorder that results in frequent night-time awakenings and daytime sleepiness), decreased testicular size, increase in red blood count and decreased sperm count. It does not, however, cause prostate cancer.
Lately, the medical world was alarmed by two controversial studies stating that Testosterone Replacement Therapy increases heart attack and stroke risks. However, the analysis showed that there were several serious discrepancies in the studies. The discrepancies were so severe that the International Society of Sexual Medicine had issued a statement challenging their conclusions.
Twenty-five medical societies have joined the Androgen Study Group to petition the journal to retract the misleading Testosterone study. Men diagnosed with Testosterone deficiency should consider TRT after a full discussion with their healthcare provider. TRT can provide significant benefits for men with sexual dysfunction, and also for a variety of non-sexual symptoms.
Like all medical treatments, Testosterone therapy is associated with risks and should be discussed with one’s health care provider. Caution is required for those with sleep apnea, congestive heart failure, symptoms consistent with lower urinary tract obstruction, and personal or family history of prostate or breast cancer.
Methods of Testosterone Delivery
Q: How is Testosterone delivered into the body?
A: Testosterone can be administered into the body in several ways. The most common method is intramuscular (IM) injection with a syringe. Other delivery methods include transdermal application through the gel, cream, or patch applied to the skin; orally by swallowing tablets (this method is uncommon as it has  been shown to have adverse effects on the liver); sublingually/buccally by dissolving a tablet under the tongue or against the gums; or by a pellet inserted under the skin.
been shown to have adverse effects on the liver); sublingually/buccally by dissolving a tablet under the tongue or against the gums; or by a pellet inserted under the skin.
The Testosterone delivery method used will depend on the type of medication available in the country of treatment, the health risks/benefits for the patient, personal preference, and cost. Testosterone is not stored by the body for future use, so to maintain healthy levels, it must be administered at timed intervals and appropriate dosages.
Injectable and subcutaneous Testosterone pellets remain active in the body the longest. Injectable Testosterone is usually administered between once a week to once every three weeks, and subcutaneous Testosterone pellets are replaced every 3-4 months. Transdermal Testosterone (patch, gel, or cream) is typically applied to the skin in smaller daily doses; oral and sublingual/buccal Testosterone are also usually taken daily.
What if I Don't Like Needles?
Transdermal application is also attractive to those individuals who are apprehensive about needles and injections. However, there are some disadvantages to transdermal delivery. Some forms of daily transdermal Testosterone application, particularly the patch, are substantially more expensive than injectable Testosterone.
Testosterone patches often cause skin irritation or allergic reactions to users. They can fall off with excessive sweating, and they must be fully protected with plastic when swimming.
Testosterone cream and gel can be transferred by direct skin contact with a partner; special care must be taken with female partners who wish to avoid  potential masculine effects.
potential masculine effects.
There are currently two brand-name Testosterone patches available in the United States: "Androderm" and "Testoderm." (Note that there are two forms of Testoderm available: a scrotal patch and a non-scrotal patch. The non-scrotal patch, "Testoderm TTS," is described herein). Generic Testosterone patches are not yet available.
Both Androderm and Testoderm TTS are very fast-acting once they have permeated the skin. The Testosterone in the patches is suspended in an alcohol-based gel. To deliver Testosterone efficiently into the body, chemical enhancers are added to the patch to increase the absorption rate.
It is these enhancers that are often the cause of skin irritation in many users. Some individuals find Testoderm TTS to be less irritating to the skin than Androderm, but this will vary from person to person.
What About Testosterone Creams and Gels?
Creams and gels are applied directly to the skin. As mentioned earlier, care must be taken to avoid skin-to-skin contact with a partner on the site of the application. Transfer of the Testosterone from the site can be prevented by keeping the area covered.
To avoid transfer to another person, clothing should be worn to cover the application sites. If direct skin-to-skin contact with another person is anticipated, the application sites should be washed thoroughly with  soap and water.
soap and water.
Users should wait at least 2 hours after applying before showering or swimming; for optimal absorption, it may be best to wait 5-6 hours. All creams and gels should be applied to clean, dry skin -- preferably to the shoulders and upper arms.
It should not be applied to the genitals or the abdomen. Application sites should be allowed to dry for a few minutes before dressing. Finally, don't forget to wash your hands thoroughly with soap and water after use.
Contact us for a FREE, no-obligation discussion concerning the benefits of testosterone restoration.
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- LabCorp Announces a Change to the Testosterone Reference Range [Last Updated On: April 16th, 2025] [Originally Added On: June 23rd, 2019]
- Important Facts About Testosterone Therapy Before Buying [Last Updated On: April 18th, 2025] [Originally Added On: July 13th, 2019]
- Soy: Does it Lower Testosterone? [Last Updated On: October 18th, 2024] [Originally Added On: August 30th, 2020]
- Testosterone Treatments May Successfully Reverse Type-2 Diabetes in Some Men [Last Updated On: April 15th, 2025] [Originally Added On: November 13th, 2020]
- Testosterone Replacement Therapy (TRT) May Prevent Heart Attacks and Diabetes [Last Updated On: April 21st, 2025] [Originally Added On: November 17th, 2020]
- Did You Know? Recent Studies Have Confirmed the Link Between Low Testosterone (“Low-T”) and Depression. [Last Updated On: April 17th, 2025] [Originally Added On: January 10th, 2021]
- New Study Finds Testosterone Does Not Increase Your Heart Attack Risk [Last Updated On: April 14th, 2025] [Originally Added On: January 11th, 2021]
- The Great Testosterone Debate [Last Updated On: April 20th, 2025] [Originally Added On: January 14th, 2021]
- Testosterone Replacement Therapy Lowers Heart Attack Risk [Last Updated On: April 19th, 2025] [Originally Added On: January 18th, 2021]
- New Study Says: The Benefits of Testosterone Replacement Therapy Outweigh The Risks [Last Updated On: April 22nd, 2025] [Originally Added On: January 19th, 2021]
- Male Menopause. Fact or Fiction ? [Last Updated On: April 23rd, 2025] [Originally Added On: January 20th, 2021]
- Testosterone: How Much Do You Really Know About This Masculine Hormone? [Last Updated On: October 6th, 2024] [Originally Added On: February 9th, 2021]
- Low-T: What are healthy levels of Testosterone and why is it difficult to measure? [Last Updated On: September 11th, 2025] [Originally Added On: April 3rd, 2021]
- Testosterone Therapy May Be Good for the Heart if You Have Low-T [Last Updated On: May 3rd, 2025] [Originally Added On: July 21st, 2021]
- A Recent Study Concludes: Testosterone DOES NOT Cause Prostate Cancer [Last Updated On: September 14th, 2025] [Originally Added On: August 16th, 2021]
- In the Battle Against Aging, When do the Risks Outweigh the Rewards? [Last Updated On: April 4th, 2025] [Originally Added On: August 18th, 2021]
- New Study Concludes: Boosting Testosterone Levels Lowers Men's Death Risk [Last Updated On: May 11th, 2025] [Originally Added On: August 20th, 2021]
- Testosterone Replacement Therapy Slows Prostate Cancer! [Last Updated On: April 2nd, 2025] [Originally Added On: September 13th, 2021]
- Research proves that Testosterone Therapy Boosts Fertility! [Last Updated On: April 5th, 2025] [Originally Added On: September 26th, 2021]
- Free Testosterone and Sex Hormone-Binding Globulin [Last Updated On: April 6th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone Does Not Cause Heart Attacks [Last Updated On: April 7th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Women [Last Updated On: April 8th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Metabolic Syndrome [Last Updated On: April 3rd, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Disease Prevention [Last Updated On: March 31st, 2025] [Originally Added On: October 15th, 2021]
- Judge Vacates $140 Million Verdict in Testosterone Lawsuit [Last Updated On: April 1st, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Estrogen [Last Updated On: April 9th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Aging [Last Updated On: April 10th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Replacement Therapy (TRT) Benefits [Last Updated On: April 11th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Male Menopause [Last Updated On: March 30th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Battles Obesity [Last Updated On: March 29th, 2025] [Originally Added On: October 16th, 2021]
- Why You Need Testosterone Replacement Therapy [Last Updated On: May 14th, 2025] [Originally Added On: October 16th, 2021]
- How Testosterone Impacts Sexual Preferences In Men and Women [Last Updated On: March 28th, 2025] [Originally Added On: October 30th, 2021]
- Growth Hormone and The Thyroid Gland [Last Updated On: April 24th, 2025] [Originally Added On: November 19th, 2021]
- How Does Masturbation Affect Testosterone Levels? Exploring the Science [Last Updated On: May 24th, 2025] [Originally Added On: March 27th, 2022]
- Testosterone Therapy Increasingly Used to Help Men Take Control of Aging [Last Updated On: May 25th, 2025] [Originally Added On: May 30th, 2022]
- The many benefits of Testosterone Replacement Therapy (TRT) [Last Updated On: November 1st, 2025] [Originally Added On: June 13th, 2022]
- Tlando Testosterone - A Brand New Way to Treat Low-T Safely with a Testosterone Pill [Last Updated On: May 28th, 2025] [Originally Added On: July 12th, 2022]
- Safe Tlando Testosterone Changes Landscape of Low-T Therapy [Last Updated On: May 30th, 2025] [Originally Added On: August 15th, 2022]
- Systems to Monitor Testosterone Replacement Therapy (TRT) [Last Updated On: October 12th, 2025] [Originally Added On: September 21st, 2022]
- Testosterone May Help You Keep Your Job (Or Find Another) [Last Updated On: June 12th, 2025] [Originally Added On: October 4th, 2022]
- Toxic Chemicals are Killing your testosterone…And your Manhood! [Last Updated On: October 28th, 2024] [Originally Added On: October 10th, 2022]
- A new study reveals that Testosterone improves body composition in men with low testosterone! [Last Updated On: October 22nd, 2025] [Originally Added On: October 17th, 2022]
- A former Mr. Olympia speaks about testosterone [Last Updated On: October 10th, 2025] [Originally Added On: November 8th, 2022]
- Testosterone Blockers Thwart Melanoma [Last Updated On: June 9th, 2025] [Originally Added On: December 11th, 2022]