Video Link: https://vimeo.com/279256674
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
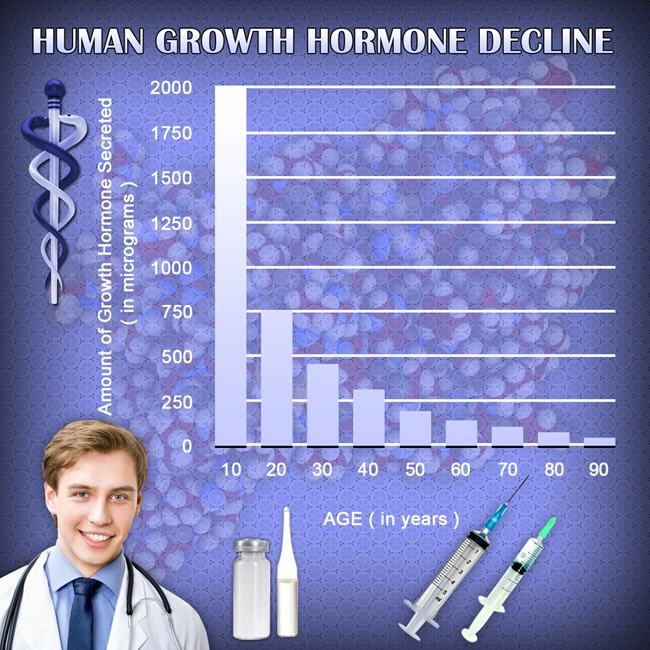
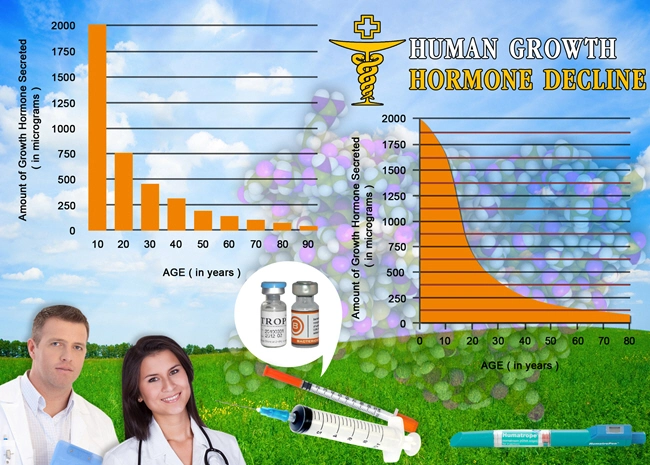
At our clinic, we are proud to offer the most systemized, streamlined, and safe hormone replacement therapy. Our menu includes Testosterone Replacement Therapy (TRT), Human Growth Hormone (HGH) Replacement Therapy, and Sermorelin replacement therapy. Before we begin treatment we ensure that you are able to benefit from our treatment regimens, and that includes a brain scan to detect levels of Aromatase.
Aromatase is nn enzyme that transforms testosterone to estrogen seems to have a significant impact on both a healthy and injured brain, according to a recent report
 There is a growing body of evidence that in the healthy brain, aromatase, and the estrogen that makes it possible for neurons to produce, help keep our minds sharp and flexible. Scientists have discovered that when injury occurs, aromatase and estrogen manifestation seems to shift to cells in the brain named astrocytes.
There is a growing body of evidence that in the healthy brain, aromatase, and the estrogen that makes it possible for neurons to produce, help keep our minds sharp and flexible. Scientists have discovered that when injury occurs, aromatase and estrogen manifestation seems to shift to cells in the brain named astrocytes.
These cells support and nurture stressed brain neurons, said Dr. Darrell Brann, Regents' Professor and Vice Chairman of the Department of Neuroscience and Regenerative Medicine at the Medical College of Georgia at Georgia Regents University.
Numerous studies, including those in Brann's lab, have demonstrated this shift in aromatase/estrogen expression from neurons to astrocytes after injury.
In Brann's case, the studies have focused on the hippocampus, a center of learning, memory, and emotions. Inflammation and brain damage occurred after he used a drug to lower the expression of aromatase in that area.
A $1.8 million grant from the National Institute of Health will allow him to continue his research into the role of aromatase and estrogen in injury and health and possibly find treatments that can build up the brain's effort to heal.
The research is being conducted with laboratory mice, one with aromatase removed from neurons, another with it missing in astrocytes, and a third with aromatase deficient in both brain cell types.
aromatase deficient in both brain cell types.
The mice were grown by Brann's lab in collaboration with Dr. Ratna K. Vadlamudi, Professor of Obstetrics and Gynecology at the University of Texas Health Sciences Center.
"We will be able to tell the cell-specific function of estrogen," Brann said. "We want to know what happens when they don't have it. We'll study the plasticity, the connectivity of neurons in these knockouts, and we'll consider their cognitive function using behavioral tests."
They'll also see what effect it has on inflammation and recovery when aromatase expression can't multiply as it normally does after injury.
Brann is not dumbfounded that normally supportive astrocytes levels would surge after injury and believes estrogen is crucial to the expanded role.
"In a non-injury situation, we see it mostly in the neurons, so it much [sic] has some functions such as plasticity and connectivity normally," he said.
After an injury occurs, and astrocytes begin pumping out aromatase then estrogen, the focus seems to shift to protection and recovery.
He added that astrocyte support is not iron-clad; at times, natural recovery mechanisms get crushed by the extent of the damage.
However, Brann hopes that the new studies will lead to new therapies that assist the natural recovery effort.
Neurons express aromatase in a healthy hippocampus.
Subsequent to a traumatic injury or stroke, the elevated expression seems to shift to astrocytes, a type of glial cell, found in abundance in the central nervous system that supports and cushions neurons.
Astrocytes become more active following brain trauma, unleashing more protective, restorative factors that scientists believe help tamper down inflammation and boost their protection of neurons.
 However, if astrocytes stay stimulated for too long, they may cause problems, including gliosis, which is mainly a scar-like wad of glial cells in the region living neurons previously occupied.
However, if astrocytes stay stimulated for too long, they may cause problems, including gliosis, which is mainly a scar-like wad of glial cells in the region living neurons previously occupied.
"You have to regulate all these factors being released tightly," Brann said.
Even in culture, neurons will connect and communicate, but scientists add an aromatase inhibitor to the equation, which halts connectivity.
A few of the initial in vivo studies in zebra finches determined that aromatase levels surged after a brain injury, which also proves a protective role for the protein. More brain damage happens when aromatase inhibitors are given.
"There seemed to be more inflammation," Brann said.
Brann wants to explore whether estrogen regulates brain-derived neurotrophic factor, which plays a role in brain plasticity and connectivity.
He also plans to delve into the role of aromatase and estrogen in neurodegenerative diseases, such as Alzheimer's, where there is some indication that missing aromatase increases plaque development.
Naturally high estrogen levels in premenopausal women are considered to be protective of stroke as well as heart attacks and other maladies.
The link between hormones and traumatic brain injury
Numerous studies have demonstrated that hormonal imbalances are linked to traumatic brain injury (TBI). Hypopituitarism (a disease where the pituitary gland manufactures healthy growth hormone levels) is quite common following brain injuries – as high as two-thirds to one-half of those patients.
The worst part of this heartbreaking development is that the hormone deficiency may lie undetected for decades following the trauma. Tragically, this makes a bad situation far worse, as the brain deterioration and memory loss continue to increase unchecked.
But why? Why does this happen? Why would damage to the brain result in hormone levels going into a free-fall?
To answer those questions, we need to start with the pituitary gland. Often referred to as “the master gland” the pituitary is the command center of other endocrine glands.
However, the pituitary is controlled by the hypothalamus gland. The hypothalamus monitors the pituitary by telling the gland how much of its hormones to release.
The hypothalamus then receives feedbacks by neurological input from virtually all of the body. This process is crucial to maintaining hormonal balance.
Knowing this connection, it is now apparent that damage to the brain, even in small amounts, can wreak havoc on the hypothalamic-pituitary system and have devastating consequences on our hormonal equilibrium.
In fact, it is the unsettling of the hormonal system that plays a huge role in the broad range of neurological problems of TBI, not the brain injury itself.
The hormone estradiol plays a critical role in the growth of neurons by both decreasing inflammation and promoting the growth of dendrites.
Dendrites resemble tree branches sprouting from the ends of neurons that receive signals from other neurons and send electrical stimulation to the heart of the attached neuron.
Testosterone is converted to estradiol in men’s brains when aromatase is present, and this helps to lessen the impact of the brain injury.
Studies have concluded that low levels of estradiol are lower cognition scores in both men and women.
Conversely, healthy testosterone levels boosted scores on the Mini-Mental Status Examination. Other studies have arrived at similar conclusions. Also, recovery from TBI occurs more often in patients with high testosterone levels.
Hormone Replacement Therapy (HRT) and prevention of dementia
This is, of course, no guarantee that dementia, mild cognitive impairment (MCI) and Alzheimer’s Disease (AD) can be prevented.
However, every one of the above-mentioned brain disorders has one thing in common: diminished hormone levels. Healthy hormone levels can provide a degree of protection from these dreaded mind afflictions.
But this could become a case of “too much of a good thing.” Studies have concluded that there may be a “golden mean” level of hormones where more may negate the benefits that HRT can deliver.
The key is to measure and monitor to determine that hormonal “sweet spot.”
And that’s why you need to contact us
A grim, sad fact: most hormonal deficiencies are not even identified, let alone treated. Despite the growing mountain of evidence that has established a direct link between low hormone levels and TBI, very few doctors are considering HRT for treatment of the injured brain.
But we do! At our clinic, our main priority is to ensure that your hormones are at optimal levels...not too high and not too low. We have the experienced to determine precisely the dosage that will give the maximum benefit to your entire body – and that includes your mind as well.
Considering the association of low hormones with brain impairment, it is recommended that everyone, not just people dealing with TBI, undergo hormone testing.
Contact us for a FREE no-obligation consultation.
References
https://en.wikipedia.org/wiki/Aromatase
https://medicalxpress.com/news/2015-05-enzyme-testosterone-estrogen-big-role.html
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Why Do Women Develop Alzheimer’s and Cognitive Decline More Than Men? Hormones Might Be the Reason [Last Updated On: August 30th, 2025] [Originally Added On: May 10th, 2021]
- Testosterone Replacement Therapy Boosts Memory! [Last Updated On: May 16th, 2025] [Originally Added On: September 13th, 2021]
- Growth Hormone and Stress Reduction [Last Updated On: March 16th, 2025] [Originally Added On: October 14th, 2021]
- Matching Sex Drives Are Important to a Healthy Relationship [Last Updated On: June 10th, 2025] [Originally Added On: November 23rd, 2022]