Video Link: https://vimeo.com/286620204
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Testosterone: The Master Protector
Keep reading and discover how testosterone’s many benefits just keep on coming!
The benefits of testosterone are well-known: increased strength and muscle mass; surging energy levels; lower blood pressure and cholesterol levels,  deeper, more restorative sleep, and sharpened mental function.
deeper, more restorative sleep, and sharpened mental function.
But There are Other, Lesser-Known Benefits of Testosterone
That’s right. Did you know:
Testosterone can help men who are suffering from osteoporosis.
Testosterone may protect men from Asthma attacks.
Testosterone Replacement Therapy (TRT) is both efficient and safe if done correctly under medical supervision.
Testosterone has been linked to lowering cholesterol and insulin levels.
Let’s take a more in-depth look at each one of these benefits.
There is a common misconception that men don’t have to be concerned about developing osteoporosis.
The definition of osteoporosis is “a medical condition in which the bones become brittle and fragile from loss of tissue, typically as a result of hormonal changes, or deficiency of calcium or vitamin D.”
The crucial words in that definition are “hormonal changes.” The fact is, that as a man’s testosterone levels drop, his risk of osteoporosis rises.
For proof of this fact, it has been demonstrated that young men who suffer from low testosterone due to a congenital condition or unusual medical issue also have weakened bones.
For these young men, TRT has been just what the doctor ordered. Studies have shown that a mere one year of TRT has boosted their bone density.
Additional Studies Looked at the Effectiveness of TRT in Older Men
In a 1996 study, 36 men with a median age of 58 who suffered from low testosterone levels were given three separate tests at three different times. The men received regular testosterone injections on schedule for 18 months.
The study concluded that the men experienced increased bone density in the spine by up to 5 percent. As a bonus, the men lost fat and gained muscle.
 A second study in 2004 looking at testosterone’s effect on older men’s bone density involved 48 men with testosterone levels below 350 nanograms per deciliter (ng/dL), which is considered low by all standards.
A second study in 2004 looking at testosterone’s effect on older men’s bone density involved 48 men with testosterone levels below 350 nanograms per deciliter (ng/dL), which is considered low by all standards.
Twenty-four of the study participants received testosterone injections of 200 milligrams every two weeks for three years.
The remaining 24 men received a placebo injection every two weeks.
When the study concluded, the men who received testosterone experienced more than a 9% improvement in spinal bone density, but minimal improvement in hip bone density.
The placebo group experienced no change in either spinal or hip bone density.
A third study on testosterone and bone density conducted in 2017 consisted of 211 men over the age of 65 with an average age of 72. The men had deficient testosterone levels (below 275 ng/dL).
The participants were treated with AndroGel, which is a topical gel applied to the skin. The dosage was 5 grams applied to the skin daily for one year. A control group used a placebo gel.
Both groups were also given supplemental calcium and vitamin D.
At the end of the year, the men who received testosterone experienced a 7.5 per cent increase in bone density of the spine and a 3.3 per cent increase in bone density of the hip.
In the placebo group, the men showed an increase of a mere 0.8 per cent in spinal bone density and a 2.1 per cent increase in hip bone density.
The conclusion to be drawn from these studies appears obvious. Men who are stricken with osteoporosis and low testosterone should seriously consider testosterone replacement therapy.
And not just for stronger bones. Keep reading and unearth more potential benefits of TRT.
Testosterone is Linked to Lower Cholesterol and Insulin Levels
A 2016 study demonstrated that older men with low testosterone who were treated with a topical testosterone gel for one year experienced slight drops in their cholesterol and insulin levels.
A similar group of men were treated with a placebo gel and saw no changes in their cholesterol and insulin levels.
No changes were seen in the measures of fibrinolysis (the enzymatic break down of the fibrin in blood clots), inflammation, or heart damage in the study participants.
 “The effects of testosterone treatment on cardiovascular risk is uncertain,” said Emile R. Mohler III, MD, of the division of cardiovascular disease at the University of Pennsylvania Perelman School of Medicine.
“The effects of testosterone treatment on cardiovascular risk is uncertain,” said Emile R. Mohler III, MD, of the division of cardiovascular disease at the University of Pennsylvania Perelman School of Medicine.
He added “Some retrospective studies using electronic medical records have reported more cardiovascular adverse events in men taking testosterone than in men not taking it, but others have not. ... Meta-analyses of clinical trials have generally not shown more adverse cardiovascular events in men taking testosterone than in men taking a placebo, but none of the individual trials was designed prospectively to capture these events.”
788 men with a minimum age of 65 and with testosterone levels of 275 ng/dL or lower participated in seven double-blind, placebo-controlled trials created to determine the efficiency of TRT in men with low testosterone (“Low-T”) due to aging.
The men received a daily dose of 5 grams of 1% testosterone gel (AndroGel, AbbVie) or a placebo for one year.
The participants were given blood tests at the beginning of the study (baseline) and 3, 6, 9 and 12 months. The blood work measured glucose concentration, serum insulin levels, lipid profile, HbA1c, C-reactive protein, D-dimer, and troponin 1.
The Results of the Study
After one year, lipid levels dropped in both the testosterone and placebo groups. However, after an adjustment for the baseline levels, the testosterone group showed an average of 6.1 mg/dL drop in total cholesterol as compared to the placebo group.
The testosterone subjects also saw a reduction in both HDL cholesterol (adjusted difference, -2 mg/dL; P,.001) and LDL cholesterol (adjusted difference, -4.2; P=.005) compared to the placebo group.
The changes in LDL cholesterol were somewhat more significant in the testosterone group, and there were no substantial differences in triglyceride levels.
Testosterone caused somewhat lower fasting insulin levels (adjusted mean difference, - 1.7 IU/mL; P = .02) and homeostatic model assessment of insulin resistance (adjusted mean difference, -0.6; P= .03) when compared to the placebo group.
There were no changes in the levels of D-dimer, C-reactive protein, interleukin-6, troponin, glucose, or HbA1c in both groups.
The researchers determined that the importance of the lower cholesterol levels in the testosterone group is uncertain since both HDL and LDL levels dropped, as did insulin and HOMA-IR.
as did insulin and HOMA-IR.
The researchers concluded that “In the 138 men in the T Trials who underwent CT angiography at baseline and month 12, testosterone treatment was associated with a more significant increase in non-calcified coronary artery plaque volume than placebo treatment; yet in all T Trial participants, a similar number of men (seven) in each treatment arm experienced significant adverse cardiovascular events.
A trial of a much larger number of men treated for a much longer time would be necessary to determine if testosterone treatment of hypogonadal men affects clinical cardiovascular risk.”
Testosterone research will continue. Another study determined that testosterone may offer men protection from a severe lung condition.
Testosterone May Protect Men From Asthma
A recent study, funded by grants from the National Institute of Health and the U.S. Department of Veterans Affairs (VA) and published in the journal Cell Reports, concluded that testosterone might help shield men from the debilitating and painful effects of asthma.
If confirmed and proven, this link may explain why women are more apt to suffer from asthma than men.
In the study, researchers observed a protein in lung inflammation and discovered that testosterone lowered its production in mouse cells in the lab.
By contrast, female hormones (estrogen and progesterone) did not have a significant impact.
The different gender hormones have long been suspected of playing a role in the development of asthma.
Strangely, boys in childhood suffer from higher rates of asthma than girls. In adulthood the exact opposite occurs; women have higher rates of the disease than men.
According to Dawn Newcomb, the lead author of the study, "This change occurs around puberty, making us interested in how sex hormones are regulating inflammation with asthma."
Newcomb is a research assistant professor of medicine at Vanderbilt University.
In other lab animal studies, researchers have discovered that estrogen ramps up airway inflammation while testosterone lowers it. As with all animal studies, this does not mean that the same thing occurs in humans. But this result does add to a growing stack of evidence that points toward the association of hormones and asthma in adults.
Testosterone’s Effect on ILC2 Cells
In the study, Newcomb and her colleagues examined blood samples from both men and women, with and without asthma. Specifically, they were looking for cells that assist in making the proteins involved in lung inflammation and mucus creation.
They discovered that women with asthma had double the number of ILC2 cells circulating in their blood compared to men with the condition.
 Next, they added testosterone to the ILC2 cells. This addition diminished the cell's manufacture of the proteins that caused lung inflammation. When they added the hormones estrogen and progesterone, there was no substantial impact.
Next, they added testosterone to the ILC2 cells. This addition diminished the cell's manufacture of the proteins that caused lung inflammation. When they added the hormones estrogen and progesterone, there was no substantial impact.
Dr. Norman Edelman, senior scientific advisor to the American Lung Association and a professor at Stony Brook University, says that while the results of this new study are encouraging, it may not explain everything needed to treat the disease effectively.
"I don't think anybody would claim this is the reason for the whole difference between males and females," he said.
However, he says it's still compelling evidence that partly explains the disparity.
There are, of course, several different factors that contribute to asthma, and some of those factors may account for the gender differences in the condition.
Obesity is one of those factors, and women are more apt to be obese than men. Also, there are other possible causes of asthma, such as how nerve cells respond to airway constriction.
These factors need further investigation.
In spite of these other possible causes, professor Newcomb is hopeful that the results of this study can spearhead new treatment approaches.
"I think the findings could be applied as we, as an asthma community, are trying to develop better therapeutics for patients with asthma," she stated.
For instance, in experimenting with therapeutics that change ILC2 cell function, it may be useful to know that there may be differences between the sexes.
Dr. Edelman added that biological discoveries like this could “open up avenues for new approaches to therapy.”
However, Caution is Still Warranted with Testosterone Replacement
Testosterone replacement therapy is shrouded in controversy, as are virtually all crucial medical issues, treatments, and topics.
There is a good reason for this controversy. Medical research continues, new information and evidence appear, and the data used is not always easy to interpret.
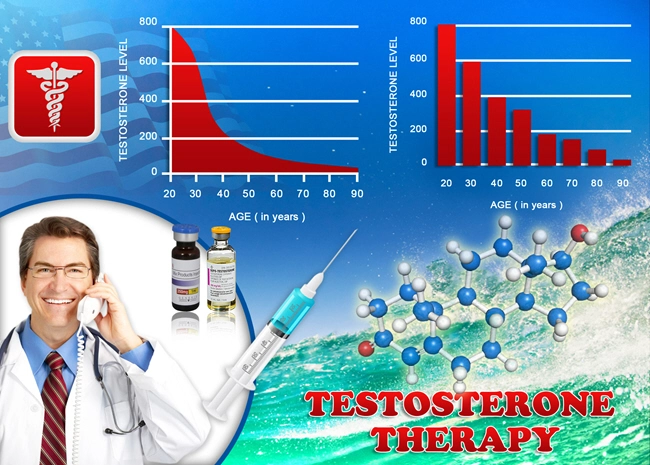
There is universal agreement on the fact of the gradual decline of testosterone in aging men. However, there is no widespread consensus as to what, if anything, to do about it.
When testosterone therapy is administered, there is the possibility of the treatment disrupting the “pituitary-testicular axis.” This axis is the highway of the endocrine system, both for messages and feedback loops.
When receiving TRT the body senses that there is no need to continue to manufacture the hormone and testosterone production goes on strike. This development can result in several unwanted side effects such as reduced sperm count and shrunken testicles.
 Also, the US Food and Drug Administration has issued warnings of an increased risk of cardiovascular problems and stroke in older men undergoing TRT.
Also, the US Food and Drug Administration has issued warnings of an increased risk of cardiovascular problems and stroke in older men undergoing TRT.
There is also a concern about men using testosterone gel and inadvertently exposing testosterone to women and children.
The consequences of this exposure could be ugly: for children, the results could be an abnormal growth of sex organs, early puberty, excessive aggression, and surging libidos.
Women coming into accidental contact with testosterone gel could experience acne and hirsutism (excessive body hair). If a woman is pregnant, she could pass on masculine traits to a female fetus.
But You Won’t Have to Worry About These Side Effects
The vast majority of incidences of the side effects just mentioned occurred when men self-treated with TRT under no professional medical supervision.
As a consequence of going it alone, they were unaware of the proper, safe methods of TRT protocol. And the results were troublesome and possibly disastrous.
Don’t let this happen to you. Don’t try this at home. We have the experience, the know-how, and the credentials to deliver the benefits of testosterone in a safe, efficient manner.
References
Testosterone therapy provides protection against cardiovascular disease in men with low testosterone
Testosterone Replacement Therapy May Protect Against Stroke, Heart Attack in Hypogonadism
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- LabCorp Announces a Change to the Testosterone Reference Range [Last Updated On: April 16th, 2025] [Originally Added On: June 23rd, 2019]
- Important Facts About Testosterone Therapy Before Buying [Last Updated On: April 18th, 2025] [Originally Added On: July 13th, 2019]
- Soy: Does it Lower Testosterone? [Last Updated On: October 18th, 2024] [Originally Added On: August 30th, 2020]
- Testosterone Treatments May Successfully Reverse Type-2 Diabetes in Some Men [Last Updated On: April 15th, 2025] [Originally Added On: November 13th, 2020]
- Testosterone Replacement Therapy (TRT) May Prevent Heart Attacks and Diabetes [Last Updated On: April 21st, 2025] [Originally Added On: November 17th, 2020]
- Did You Know? Recent Studies Have Confirmed the Link Between Low Testosterone (“Low-T”) and Depression. [Last Updated On: April 17th, 2025] [Originally Added On: January 10th, 2021]
- New Study Finds Testosterone Does Not Increase Your Heart Attack Risk [Last Updated On: April 14th, 2025] [Originally Added On: January 11th, 2021]
- The Great Testosterone Debate [Last Updated On: April 20th, 2025] [Originally Added On: January 14th, 2021]
- Testosterone Replacement Therapy Lowers Heart Attack Risk [Last Updated On: April 19th, 2025] [Originally Added On: January 18th, 2021]
- New Study Says: The Benefits of Testosterone Replacement Therapy Outweigh The Risks [Last Updated On: April 22nd, 2025] [Originally Added On: January 19th, 2021]
- Male Menopause. Fact or Fiction ? [Last Updated On: April 23rd, 2025] [Originally Added On: January 20th, 2021]
- Testosterone: How Much Do You Really Know About This Masculine Hormone? [Last Updated On: October 6th, 2024] [Originally Added On: February 9th, 2021]
- Low-T: What are healthy levels of Testosterone and why is it difficult to measure? [Last Updated On: September 11th, 2025] [Originally Added On: April 3rd, 2021]
- Testosterone Therapy May Be Good for the Heart if You Have Low-T [Last Updated On: May 3rd, 2025] [Originally Added On: July 21st, 2021]
- A Recent Study Concludes: Testosterone DOES NOT Cause Prostate Cancer [Last Updated On: September 14th, 2025] [Originally Added On: August 16th, 2021]
- In the Battle Against Aging, When do the Risks Outweigh the Rewards? [Last Updated On: April 4th, 2025] [Originally Added On: August 18th, 2021]
- New Study Concludes: Boosting Testosterone Levels Lowers Men's Death Risk [Last Updated On: May 11th, 2025] [Originally Added On: August 20th, 2021]
- Testosterone Replacement Therapy Slows Prostate Cancer! [Last Updated On: April 2nd, 2025] [Originally Added On: September 13th, 2021]
- Research proves that Testosterone Therapy Boosts Fertility! [Last Updated On: April 5th, 2025] [Originally Added On: September 26th, 2021]
- Free Testosterone and Sex Hormone-Binding Globulin [Last Updated On: April 6th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone Does Not Cause Heart Attacks [Last Updated On: April 7th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Women [Last Updated On: April 8th, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Metabolic Syndrome [Last Updated On: April 3rd, 2025] [Originally Added On: October 15th, 2021]
- Judge Vacates $140 Million Verdict in Testosterone Lawsuit [Last Updated On: April 1st, 2025] [Originally Added On: October 15th, 2021]
- Testosterone and Estrogen [Last Updated On: April 9th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Aging [Last Updated On: April 10th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Replacement Therapy (TRT) Benefits [Last Updated On: April 11th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone and Male Menopause [Last Updated On: March 30th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone Battles Obesity [Last Updated On: March 29th, 2025] [Originally Added On: October 16th, 2021]
- Why You Need Testosterone Replacement Therapy [Last Updated On: May 14th, 2025] [Originally Added On: October 16th, 2021]
- Testosterone FAQ's [Last Updated On: May 13th, 2025] [Originally Added On: October 25th, 2021]
- How Testosterone Impacts Sexual Preferences In Men and Women [Last Updated On: March 28th, 2025] [Originally Added On: October 30th, 2021]
- Growth Hormone and The Thyroid Gland [Last Updated On: April 24th, 2025] [Originally Added On: November 19th, 2021]
- How Does Masturbation Affect Testosterone Levels? Exploring the Science [Last Updated On: May 24th, 2025] [Originally Added On: March 27th, 2022]
- Testosterone Therapy Increasingly Used to Help Men Take Control of Aging [Last Updated On: May 25th, 2025] [Originally Added On: May 30th, 2022]
- The many benefits of Testosterone Replacement Therapy (TRT) [Last Updated On: November 1st, 2025] [Originally Added On: June 13th, 2022]
- Tlando Testosterone - A Brand New Way to Treat Low-T Safely with a Testosterone Pill [Last Updated On: May 28th, 2025] [Originally Added On: July 12th, 2022]
- Safe Tlando Testosterone Changes Landscape of Low-T Therapy [Last Updated On: May 30th, 2025] [Originally Added On: August 15th, 2022]
- Systems to Monitor Testosterone Replacement Therapy (TRT) [Last Updated On: October 12th, 2025] [Originally Added On: September 21st, 2022]
- Testosterone May Help You Keep Your Job (Or Find Another) [Last Updated On: June 12th, 2025] [Originally Added On: October 4th, 2022]
- Toxic Chemicals are Killing your testosterone…And your Manhood! [Last Updated On: October 28th, 2024] [Originally Added On: October 10th, 2022]
- A new study reveals that Testosterone improves body composition in men with low testosterone! [Last Updated On: October 22nd, 2025] [Originally Added On: October 17th, 2022]
- A former Mr. Olympia speaks about testosterone [Last Updated On: October 10th, 2025] [Originally Added On: November 8th, 2022]
- Testosterone Blockers Thwart Melanoma [Last Updated On: June 9th, 2025] [Originally Added On: December 11th, 2022]