Low testosterone in men might increase the risk of severe COVID
Many people know that Testosterone Replacement Therapy (TRT) delivers many benefits: Larger muscles, increased strength, skyrocketing energy, enhanced libido, melting fat, easing joint aches and pains, better sleep, mood boost, and sharper thinking.
But did you know that TRT might protect against severe COVID-19?
That’s right. A study conducted at St. Louis University and Washington University by a team of researchers concluded that men diagnosed with hypogonadism (aka “Low-T”) were 3.6 times more likely to be hospitalized with severe illness from COVID-19 than men with normal testosterone levels.
The research team looked at the health records of 723 adult men infected with COVID to determine their testosterone levels between Jan.1, 2014, to Dec. 31, 2021. Most survey subjects had caught COVID in 2020 before the COVID vaccines were developed.
2021. Most survey subjects had caught COVID in 2020 before the COVID vaccines were developed.
The team defined low testosterone as below 175 to 300 nanograms per deciliter (ng/dl). The measurements were taken around 7 months before the COVID virus in 73% of the participants, and an average of approximately 6 months after recuperating for 27% of the men.
The results were surprising.
Here is the data on the 723 research subjects:
Average age: 55
Average Body Mass Index (BMI): 33.5 kilograms per meter squared (obese)
60% had standard testosterone levels
16% had Low-T
25% were undergoing TRT
134 men were hospitalized. These subjects were older (62 vs. 53 average age), suffered from more comorbid conditions, and were more prone to have weakened immune systems (19% vs. 4% of the non-hospitalized participants).
32 of the study participants were undergoing androgen deprivation therapy, a form of chemical castration intended to impede prostate cancer growth. This group's average testosterone level was an anemic 3.5 ng/dl. 18 of these men required hospitalization, and 3 required intensive care.
Let’s make sense of these numbers.
Without considering risk factors, the men suffering from andropause (aka male menopause, another name for Low-T) WITH COVID were 3.6 times more apt to require hospital admission for their virus treatment. The risk was 2.4 times more than the standard testosterone group when the underlying, preexisting medical problems were considered.
Subjects receiving TRT that still had Low-T were more likely to be hospitalized. But men responding to TRT favorably had a comparable risk of requiring a hospital stay as men with average testosterone levels.
After adjusting for risk factors, the Low-T group was at a slightly higher risk of hospital admission: intensive care unit (ICU) admission: 9% Low-T vs. 3% standard testosterone levels; ventilator: (4% vs. 2%), or death (4% vs. 2%). The results were consistent if testosterone levels were checked before or after the COVID contagion.
When tracking time spent in the hospital, the team divided the men into three groups: Hypogonadism,
normal testosterone levels, and those currently undergoing TRT. Here are the results with the sequence of Low-T, average T, and receiving TRT:
The average number of days hospitalized: (6 vs. 6 vs. 8 days)
ICU: (6 vs. 4 vs. 14)
On a ventilator: (14 vs. 8 vs. 12)
Why TRT is so crucial
Here is a reminder of the debilitating symptoms and effects of Low-T:
Accumulating fat, especially belly fat
Shrinking muscle
Weakened bones that may lead to osteoporosis
Chronic fatigue
Compromised immune system
Elevated blood pressure
Higher LDL cholesterol levels (The “bad cholesterol”)
Poor sleep quality
Depression
Mental fog and confusion
Increased joint aches and pains
Metabolic syndrome
Type 2 diabetes
A lower sense of well-being and reduced quality of life
Kidney disease and lung impairments
And more health issues that make men with Low-T sitting ducks for the dreaded COVID.
Some of these conditions are nearly identical to the effects of COVID. This results in a “double-whammy” for hypogonadal sufferers.
The team wrote: "Men with chronically low testosterone concentrations have decreased muscle mass and less strength, both of which contribute to reduced lung capacity and ventilator dependence. Aging and comorbid conditions, which are risk factors for hospitalization for COVID-19, are also associated with hypogonadism."
They added that testosterone therapy might ease the ferocity of COVID-19 by boosting muscle mass and strength and reducing inflammation, precisely what men with low-T need. Such therapy, however, carries an increased risk of prostate cancer and may increase the risk of heart disease.
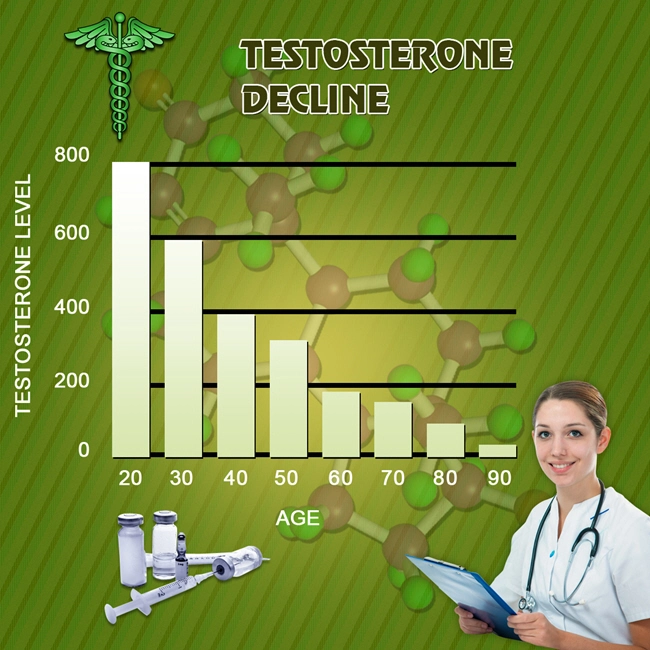
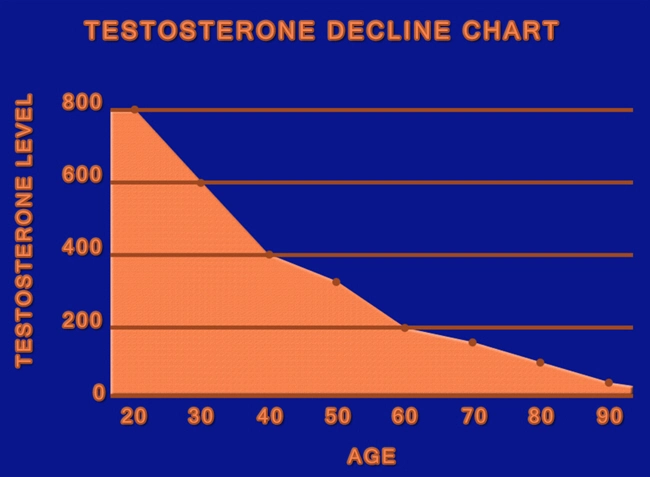
 In a Washington University press release, senior author Abhinav Diwan, MD, a professor of medicine at Washington University, stated that low testosterone is widespread and growing, affecting up to a third of men over 30. The manly hormone drops steadily at around 10% per decade if left untreated.
In a Washington University press release, senior author Abhinav Diwan, MD, a professor of medicine at Washington University, stated that low testosterone is widespread and growing, affecting up to a third of men over 30. The manly hormone drops steadily at around 10% per decade if left untreated.
“It is very likely that COVID-19 is here to stay,” according to Diwan, who added, “Hospitalizations with COVID-19 are still a problem and will continue to be a problem because the virus keeps evolving new variants that escape immunization-based immunity. Low testosterone is very common; up to a third of men over 30 have it. Our study draws attention to this important risk factor and the need to address it as a strategy to lower hospitalizations.”
Sandeep Dhindsa, MD, an endocrinologist at Saint Louis University, and co-senior author Diwan have previously found that men hospitalized with COVID-19 have unusually low testosterone levels.
However, severe sickness or traumatic accidents may temporarily lower hormone levels. Whether low testosterone is a risk factor for severe COVID-19 or a consequence of it is a subject that has not been particularly well-resolved by data from men who have already been hospitalized with the disease.
The researchers wanted to discover if individuals with chronically low testosterone levels were more prone to sickness than those with normal levels.
Low testosterone was a risk factor for COVID hospitalization, but TRT reduced that risk, as per Dhindsa. "Below 200 nanograms per deciliter, where the typical range is 300 to 1,000 nanograms per deciliter, the risk dramatically increases. Age, obesity, and other health issues that we looked at as risk factors have no bearing on this. However, the risk for those receiving therapy is as usual.”
Dhindsa says their work confirmed low counts of the hormones did mean a higher risk of hospitalization.
Diwan concluded that “In the meantime, our study would suggest that it would be prudent to look at testosterone levels, especially in people who have symptoms of low testosterone, and then individualize care.”
“If they are at really high risk of cardiovascular events, then the doctor could engage the patient in a discussion of the pros and cons of hormone replacement therapy, and perhaps lowering the risk of COVID hospitalization could be on the list of potential benefits.”
What about the risk of Testosterone Replacement Therapy?
As with all treatments, TRT is not risk-free. Two significant concerns are an increased risk of prostate cancer and heart disease. The link to heart disease has not been proven, and a clinical trial is in progress to determine if TRT causes heart problems.
The link between TRT and prostate cancer has been greatly exaggerated. The entire "testosterone causes prostate cancer" myth started in 1941 based on a study by Dr. Charles B. Huggins that turned out to be severely flawed.
Several recent studies have concluded that men with Low-T who received TRT had lower rates of prostate cancer antigen (Pca), a test used to predict prostate cancer based on a genetic analysis of cells found in urine. Other studies have concluded that severe prostate cancer is directly connected to low testosterone, contrary to long-held medical beliefs.
The conclusions of this study indicate that when applied correctly, TRT could offer significant protection from the ravages of COVID and help ease the burden of overcrowded, understaffed hospitals made worse by the COVID tsunami.
The study results were featured in JAMA Network Open.
Contact us for a FREE, no-obligation discussion concerning the benefits of Testosterone Replacement Therapy!
https://medicine.wustl.edu/news/men-with-low-testosterone-may-be-at-increased-risk-of-covid-19-hospitalization/
https://www.cidrap.umn.edu/news-perspective/2022/09/low-testosterone-men-may-raise-risk-covid-hospitalization
https://studyfinds.org/testosterone-supplements-covid/
https://www.hindustantimes.com/lifestyle/health/low-testosterone-may-make-men-more-susceptible-to-covid-19-hospitalisation-101662186206430.html
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Injectable HGH Prescriptions: Blood Testing Centers in Philadelphia, Pennsylvania [Last Updated On: August 27th, 2025] [Originally Added On: March 3rd, 2019]
- Nutropin Hgh: Hgh Hormone Product [Last Updated On: December 21st, 2024] [Originally Added On: March 10th, 2020]
- Hgh Replacement [Last Updated On: December 21st, 2024] [Originally Added On: March 14th, 2020]
- Hgh Therapy [Last Updated On: December 22nd, 2024] [Originally Added On: March 15th, 2020]
- Anti-ageing Clinics Distribute Human Growth Hormone [Last Updated On: December 25th, 2024] [Originally Added On: March 16th, 2020]
- Hgh In Forefront To Remain Young [Last Updated On: November 25th, 2024] [Originally Added On: March 18th, 2020]
- Benefits Of Hgh: Thierry Hertoghe [Last Updated On: December 23rd, 2024] [Originally Added On: April 23rd, 2020]
- Getting Started With An Hgh Program [Last Updated On: December 24th, 2024] [Originally Added On: April 25th, 2020]
- Hgh Releasers [Last Updated On: December 25th, 2024] [Originally Added On: April 26th, 2020]
- What dietary considerations should I make while on HRT, hormone replacement therapy? [Last Updated On: December 20th, 2024] [Originally Added On: May 1st, 2020]
- Hgh Dosage [Last Updated On: March 3rd, 2025] [Originally Added On: May 5th, 2020]
- Hgh Deficiency [Last Updated On: December 23rd, 2024] [Originally Added On: May 6th, 2020]
- Hgh Products Genotropin Humantrope Nutropin Saizen Serostim Omnitrope [Last Updated On: November 25th, 2024] [Originally Added On: May 8th, 2020]
- What Is Injectable Hgh Human Growth Hormone? [Last Updated On: December 22nd, 2024] [Originally Added On: May 9th, 2020]
- Introduction To Human Growth Hormone HGH [Last Updated On: December 24th, 2024] [Originally Added On: May 10th, 2020]
- Omnitrope Injections for the Treatment of HGH Deficiency [Last Updated On: June 15th, 2025] [Originally Added On: May 6th, 2021]
- Sleep To Amplify Human Growth Hormone Levels [Last Updated On: June 14th, 2025] [Originally Added On: May 27th, 2021]
- Buying Hgh Hormone Human Growth Hormone [Last Updated On: August 20th, 2025] [Originally Added On: February 22nd, 2022]
- Hgh For Menopause [Last Updated On: October 28th, 2025] [Originally Added On: February 23rd, 2022]
- Your HGH Levels [Last Updated On: October 5th, 2025] [Originally Added On: February 24th, 2022]
- Related Glossary of Terms [Last Updated On: October 14th, 2024] [Originally Added On: February 25th, 2022]
- Hgh Facts - Information About Growth Hormone [Last Updated On: August 21st, 2025] [Originally Added On: February 26th, 2022]
- Hgh Sports And Baseball [Last Updated On: August 22nd, 2025] [Originally Added On: February 27th, 2022]
- Us Olympic Committee And Talk Of Hgh [Last Updated On: October 30th, 2025] [Originally Added On: February 28th, 2022]
- Braves' Schafer Talks About His Suspension Over Hgh [Last Updated On: August 23rd, 2025] [Originally Added On: March 1st, 2022]
- Hgh Scams: Different Hgh Scams And Things To Watch For Online [Last Updated On: August 27th, 2025] [Originally Added On: March 2nd, 2022]
- Nordiflex HGH Injection Device Information [Last Updated On: October 31st, 2025] [Originally Added On: March 3rd, 2022]
- Genotropin Hgh Detailed Description [Last Updated On: October 15th, 2024] [Originally Added On: March 4th, 2022]
- Saizen Hgh Detailed Description [Last Updated On: October 17th, 2024] [Originally Added On: March 6th, 2022]
- Genotropin HGH: Human Growth Hormone Product [Last Updated On: August 24th, 2025] [Originally Added On: March 6th, 2022]
- Omnitrope Hgh: Human Growth Hormone Product Called Omnitrope. [Last Updated On: October 5th, 2024] [Originally Added On: March 7th, 2022]
- Nutropin Hgh Detailed Description [Last Updated On: November 3rd, 2025] [Originally Added On: March 8th, 2022]
- Saizen Hgh: Injectable Hgh Product [Last Updated On: August 25th, 2025] [Originally Added On: March 9th, 2022]
- Hgh Product Serostim [Last Updated On: August 26th, 2025] [Originally Added On: March 11th, 2022]
- HGH Scams (HGH Supplements) [Last Updated On: November 12th, 2024] [Originally Added On: March 20th, 2022]
- Side Effects Of HGH [Last Updated On: September 3rd, 2025] [Originally Added On: March 21st, 2022]
- Testimonial: Walter’s HGH Story [Last Updated On: September 28th, 2025] [Originally Added On: June 4th, 2022]
- HGH Is the “God Particle” [Last Updated On: September 17th, 2025] [Originally Added On: July 26th, 2022]
- Can I Reverse the Aging Process with HGH? [Last Updated On: September 19th, 2025] [Originally Added On: September 21st, 2022]
- A new study confirms: Testosterone Replacement Therapy is safe! [Last Updated On: October 4th, 2025] [Originally Added On: October 2nd, 2022]
- HGH Therapy – How Can I Know Who Is Legitimate? [Last Updated On: June 7th, 2025] [Originally Added On: January 10th, 2023]
- The Evolution of Testosterone Replacement Therapy for men with Prostate Cancer [Last Updated On: June 2nd, 2025] [Originally Added On: January 12th, 2023]
- Nine Hormones that Can Impact Your Weight and How to Promote Hormone Balance [Last Updated On: June 6th, 2025] [Originally Added On: January 26th, 2023]
- Get Tested for Hormone Levels, even if You Have No Symptoms [Last Updated On: September 29th, 2025] [Originally Added On: March 17th, 2023]
- Can Head Injuries Cause HGH Deficiency? [Last Updated On: September 26th, 2025] [Originally Added On: May 17th, 2023]
- Mountain Biker Thought his Life Was Over [Last Updated On: September 15th, 2025] [Originally Added On: May 25th, 2023]
- Do HGH Booster Supplements Work Faster Than Prescriptions? [Last Updated On: October 1st, 2025] [Originally Added On: June 3rd, 2023]
- HGH and It’s Effects on Other Hormones [Last Updated On: October 26th, 2024] [Originally Added On: June 10th, 2023]
- Maintaining a Proper Medication Schedule [Last Updated On: November 24th, 2024] [Originally Added On: August 23rd, 2023]
- What is the History of the Discovery of HGH? [Last Updated On: October 21st, 2024] [Originally Added On: September 17th, 2023]
- Don’t Let Fear Stop You From Fixing Your Hormones [Last Updated On: October 22nd, 2024] [Originally Added On: September 22nd, 2023]
- Understanding HGH Dosage [Last Updated On: February 26th, 2025] [Originally Added On: February 26th, 2025]