Video Link: https://vimeo.com/282203389
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
The Curse of Non-Alcoholic Fatty Liver Disease
No question about it: Non-alcoholic fatty liver disease (NAFLD) is indeed a curse. Liver disease often comes with a stigma of alcohol or drug abuse. But most of the people suffering from NAFLD are not problem drinkers or drug abusers.
NAFLD is Often a Result of Genetics, not a Wrong Lifestyle
That’s right. If your parents or other members of your immediate family have NAFLD, you are at high risk for the disease and need to be tested for liver function. This is true regardless of whether or not you are showing symptoms of liver dysfunction.
Never forget that liver disease is sneaky, and can remain hidden and without symptoms for decades. Then, when it strikes, a ton of damage may have already been done.
Other causes of NAFLD are high blood sugar, insulin resistance, obesity, metabolic syndrome, and the side effects of particular medications.
What is Non-alcoholic fatty liver disease?
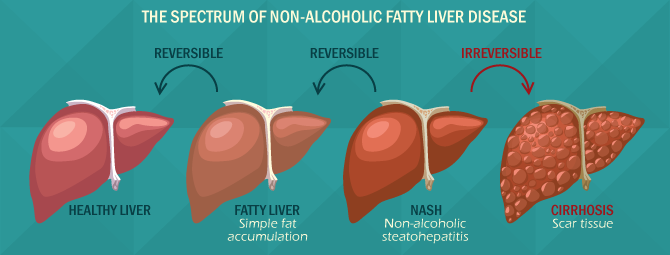
Before we continue, a definition of NAFLD is in order. Non-alcoholic fatty liver disease is the accumulation of excess fat in the liver that is not caused by alcohol. The liver always holds some fat, since processing fats are one of the liver’s many functions.
But too much fat in the liver can cause your liver to become enlarged, due to inflammation. This excess fat can lead to fibrosis (scarring) of the liver tissue. Left unchecked, fibrosis leads to cirrhosis, a severe condition that can lead to liver cancer.
Liver cancer has a five-year survival rate of 21%. Not good odds.
Other adverse health consequences occur as a result of NAFLD. Inflammation caused by excess fat in the liver may lead to atherosclerosis (hardening and narrowing of the arteries) that makes blood prone to clotting. This increases the risk of heart attack or stroke.
Also, the fatty liver disease has a direct link to diabetes. The liver plays a crucial role in regulating blood sugar. When fat accumulates in the liver, it becomes challenging for this organ to control fasting glucose levels.
challenging for this organ to control fasting glucose levels.
If that weren’t bad enough, NAFLD makes the body more insulin resistant. This condition makes the beta cells of the pancreas work harder. When combined with excess fat in the liver, this 1-2 punch sets the stage for the onset of diabetes.
What Can be Done to Stop NAFLD?
The bad news: there are currently not many medical treatments that your doctor can prescribe.
The good news. Fatty liver disease can be controlled, stopped, and even reversed! There are steps you can take immediately upon receiving the diagnosis of NAFLD. It will require a complete overhaul of your lifestyle.
However, this fact is liberating. You have a ton of control over this monstrous disease. Here are some ideas on what to do.
If you are overweight, begin to lose weight now. There is no need to go on an extreme, crash diet, or adopt a radical eating plan. There are two reasons why.
First, losing even a small percentage of your body weight can help, regardless of how much weight you need to lose. Losing weight slowly is the ticket to getting the weight off and keeping it off.
Second, as hard as it is to believe, accelerated weight-loss can make NAFLD worse, at least in the short-term. Quick weight-loss can stress the liver, which is precisely what you don’t want.
Change your relationship with sugar and simple carbohydrates. Maybe you love sugar. But sugar doesn’t love you back. Remember, NAFLD is a precursor to diabetes.
Therefore, to avoid this complication, beware of high-carbohydrate foods that cause your blood sugar to spike; specifically, lower your consumption of potatoes, rice, corn, bread, sodas, sports drinks, and juices. Better still, strive to cut them out entirely.
 Don’t be afraid of healthy fats. Olive oil, avocados, fish, walnuts, almonds, flaxseed, and Omega-3 supplements like fish oil or krill oil. Keep saturated fats to a minimum and eliminate trans-fats.
Don’t be afraid of healthy fats. Olive oil, avocados, fish, walnuts, almonds, flaxseed, and Omega-3 supplements like fish oil or krill oil. Keep saturated fats to a minimum and eliminate trans-fats.
Load up on food that delivers antioxidants: cruciferous vegetables (cauliflower, broccoli, Brussels sprouts) onions, mushrooms, garlic, berries, apples, coffee, and tea.
Consider liver-friendly supplements. Milk thistle, Alpha-lipoic-acid (ALA), Licorice root, N-acetyl-cysteine (NAC), Astragalus root, and Phosphatidylcholine (PC) have helped some people with liver issues. To be safe, discuss supplementation with your physician.
Beware of the Side Effects of Certain Medications
Some drugs have the potential to harm the liver, particularly if disease impairs your liver. Here are ten of the worst offenders that you need to keep in mind:
- Acetaminophen (Tylenol). Acetaminophen is the worst of the worst offenders. A dose exceeding four grams per day can pose problems for a healthy liver, and even more for a damaged liver.
- Seizure medications. Drugs in this category are Dilantin (phenytoin), carbamazepine, lamotrigine, and valproate.
- Azathioprine (Imuran). Azathioprine eases the effects of particular cells in your immune system. It is prescribed for autoimmune hepatitis, Crohn’s disease, and rheumatoid arthritis. Continual use can harm your liver.
- Amoxicillin Potassium Clavulanate (Augmentin). This antibiotic treats throat infections, sinus infections, and bronchitis. Before taking this medication, discuss your liver health with your doctor.
- Allopurinol (Zyloprim, Aloprim, Lopurin). Allopurinol anti-depressant to battle kidney stones and gout by lowering your body’s uric acid production. Damage to your liver is possible with Allopurinol.
- Amiodarone. If you suffer from severe arrhythmias of the heart, you may need non-steroidal Amiodarone. This drug is also used to control ventricular fibrillation, ventricular tachycardia, atrial flutter, and atrial fibrillation. If you are taking this for an extended period, make sure your liver function is monitored.
- Diclofenac (Voltaren, Cambia). This drug is a non-steroidal anti-inflammatory drug (NSAID) given to ease arthritis such as joint pain, stiffness, and swelling. Liver damage is uncommon with Diclofenac but has been known to occur. If you experience nausea, itching, yellow eyes, coca-cola colored urine, grayish stools, fatigue, and loss of appetite, check with your physician immediately.
- Methotrexate (Rheumatrex, Trexall). This substance is used in treating leukemia, psoriasis, solidified tumors, and rheumatoid arthritis. Methotrexate is linked to severe liver damage.
- Isoniazid. This drug is an antibacterial drug that prevents or treats tuberculosis. It is a well-known cause of severe liver damage. If you are prescribed this medication, do not drink alcohol.
- Risperidone (Risperdal) and Quetiapine (Seroquel). These are both antidepressant and antipsychotic drugs that can block bile flow from your liver. Bile blockage is extremely hazardous and can lead to blood toxicity.
Remember, your doctor is probably swamped with a huge caseload of patients. He or she is likely to be aware of your health condition, and would never willingly prescribe a substance that could have devastating side effects.
But it doesn’t hurt to consider yourself part of the team. Question everything prescribed to you, especially if NAFLD compromises your liver.
Get Off That Couch
Getting moving is so important in your battle against fatty liver disease. The key is to follow a well-balanced routine. Strength training (weightlifting,  bodyweight exercises), cardiovascular exercise (running, swimming, cycling) and flexibility stretching are a good foundation.
bodyweight exercises), cardiovascular exercise (running, swimming, cycling) and flexibility stretching are a good foundation.
A yoga pose called Ardha Matyendrasana - Half Lord of the Fishes Pose, is rumored to “massage the spine” and “detox the liver” which may help improve the liver’s ability to function. It is pictured here:
There are several other yoga poses that yoga practitioners claim to support the liver.
There are, however, many people who are skeptical about yoga’s liver benefits. So do your research, and consider giving yoga a try.
Another approach to consider is acupressure. Acupressure is acupuncture without needles. This means that you can “do-it-yourself.” The Lv3 pressure point shown is thought to balance the liver energy pathway, or meridian, and improve the liver’s function:
function:
As with yoga, many skeptics question the benefit of acupressure for the liver.
But both of these approaches are safe, convenient, and free. Try them, and if they help, great.
The NAFLD Curse can be Controlled
The diagnosis of non-alcoholic fatty liver disease is frightening and dreadful. But there are steps you can take to battle the scourge of NAFLD. Never forget that you are not helpless, and by taking action, you have every chance to halt the progression of this sickness and turn things around.
Of all of our organs, the liver leads the pack in its ability to regenerate. But it can’t do the job alone. Hold up your end of the deal, and give your liver the chance to heal that it deserves.
References
https://www.ncbi.nlm.nih.gov/pubmed/14685853
https://www.ncbi.nlm.nih.gov/pubmed/29272073
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- A Major Breakthrough in Anti-Aging Science is now Reality! [Last Updated On: October 12th, 2024] [Originally Added On: September 19th, 2020]
- All the Different Brands of Human Growth Hormone -- Guide [Last Updated On: February 10th, 2025] [Originally Added On: September 21st, 2020]
- Weight Loss Through HGH [Last Updated On: February 10th, 2025] [Originally Added On: September 24th, 2020]
- Did You Know: Sarcopenia is Increasing Among Senior Citizens at a Blistering Pace? [Last Updated On: February 8th, 2025] [Originally Added On: October 5th, 2020]
- Growth Hormone and Sleep [Last Updated On: February 9th, 2025] [Originally Added On: October 8th, 2020]
- Hormone Replacement Therapy Program Protocol Diary [Last Updated On: October 11th, 2024] [Originally Added On: October 9th, 2020]
- How Can I Get More HGH (Human Growth Hormone) Naturally? [Last Updated On: August 28th, 2025] [Originally Added On: August 16th, 2021]
- Cholesterol and Growth Hormone...the Truth May Surprise You! [Last Updated On: February 5th, 2025] [Originally Added On: October 7th, 2021]
- Growth Hormone FAQ's [Last Updated On: February 4th, 2025] [Originally Added On: October 8th, 2021]
- Growth Hormone: A powerful tool to battle Erectile Dysfunction [Last Updated On: February 6th, 2025] [Originally Added On: October 8th, 2021]
- How to buy Growth Hormone [Last Updated On: February 7th, 2025] [Originally Added On: October 8th, 2021]
- Testosterone Battles Diabetes [Last Updated On: February 3rd, 2025] [Originally Added On: October 8th, 2021]
- Growth Hormone protects your Adrenal Glands [Last Updated On: February 4th, 2025] [Originally Added On: October 8th, 2021]
- Buy Growth Hormone! [Last Updated On: February 9th, 2025] [Originally Added On: October 8th, 2021]
- Growth Hormone reduces Heartburn [Last Updated On: February 5th, 2025] [Originally Added On: October 8th, 2021]
- The Link Between Diabetes and Growth Hormone [Last Updated On: February 7th, 2025] [Originally Added On: October 8th, 2021]
- Growth Hormone and Nutraceuticals [Last Updated On: February 8th, 2025] [Originally Added On: October 8th, 2021]
- Growth Hormone and Depression [Last Updated On: February 3rd, 2025] [Originally Added On: October 11th, 2021]
- Growth Hormone and the Pituitary Gland [Last Updated On: February 1st, 2025] [Originally Added On: October 11th, 2021]
- Growth Hormone and Calorie Restriction. [Last Updated On: February 2nd, 2025] [Originally Added On: October 11th, 2021]
- Growth Hormone and Healthy Living Can Add Years to Your Life! [Last Updated On: February 2nd, 2025] [Originally Added On: October 11th, 2021]
- Welcome to Growth Hormone and Testosterone Therapy [Last Updated On: December 27th, 2024] [Originally Added On: October 11th, 2021]
- Human Growth Hormone Medical Guide [Last Updated On: May 18th, 2025] [Originally Added On: October 25th, 2021]
- HGH Female Blood Panel [Last Updated On: July 9th, 2022] [Originally Added On: October 28th, 2021]