Video Link: https://vimeo.com/280092871
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Andropause, also known as male menopause, is the result of a gradual drop in testosterone, which is an androgen.
The medical community is currently debating whether or not men go through a well-defined menopause.
The condition "andropause" is currently not recognized by the World Health Organization (WHO).
When andropause occurs, it is considered to be a deficiency state in which the hormone testosterone drops below the normal range for an aging male.
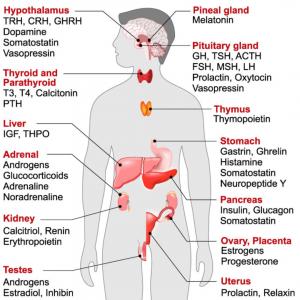
The cause of andropause is the reduction of the hormones testosterone and dehydroepiandrosterone (DHEA) in middle-aged men.
Testosterone assists the male body in building protein and is crucial for regular sexual drive and stamina.
Testosterone also contributes to several metabolic functions including bone formation and liver function.
Andropause is also associated with a decrease in Leydig cells.
A steady decline occurs in testosterone levels with age (in both men and women).
External factors that can cause testosterone levels to fall include certain forms of medication, poor diet, excessive alcohol consumption, illness, lack of sleep, lack of sex, stress, or surgery.
It can also be a symptom of neuroendocrine dysfunction after a mild traumatic brain injury.
Andropause is preceded by a condition called Hypogonadotropic Hypogonadism. A downturn in the circulation of testosterone can cause the hypothalamus and pituitary gland to trigger a release of brain hormones that stimulate the testicles to ramp up the production of testosterone.
As men age, despite low testosterone, the levels of gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH) will not rise.
The luteinizing hormone, gonadotropin-releasing hormone, and testosterone all drop below what is considered normal. Low GnRH, low LH, low testosterone  indicate the syndrome of hypogonadotropic hypogonadism, and this downward trend takes men closer to andropause.
indicate the syndrome of hypogonadotropic hypogonadism, and this downward trend takes men closer to andropause.
This phenomenon typically begins in the early forties.
Eventually, testosterone levels drop to such low levels that the hypothalamus and pituitary produce high levels of GnRH and LH to compensate.
This combination triggers the production of testosterone, which will work for a while, but then fall again.
That's when men enter andropause. They have low testosterone and a high LH and GnRH, whereas before they had low testosterone as well as low LH and GnRH.
This shift in hormonal patterns occurs in all men at some point.
The female version, a similar hormonal change that takes place in women happens in a more narrow age grouping, from the early forties to late fifties.
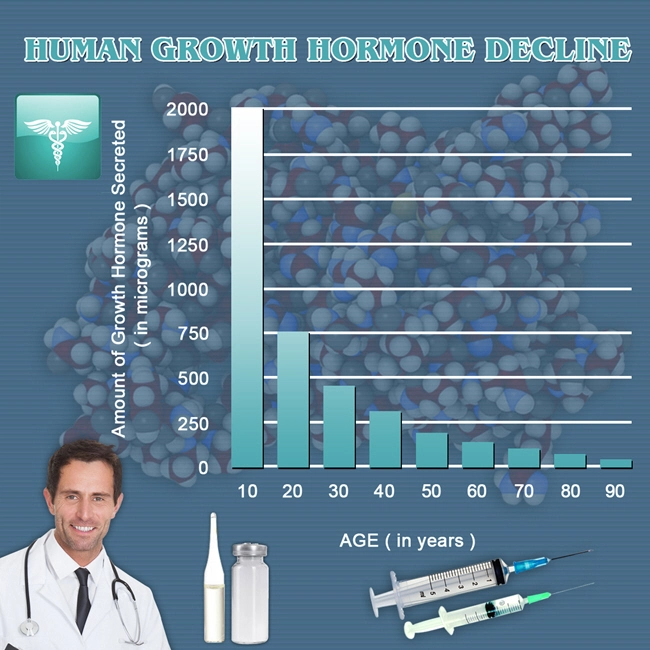
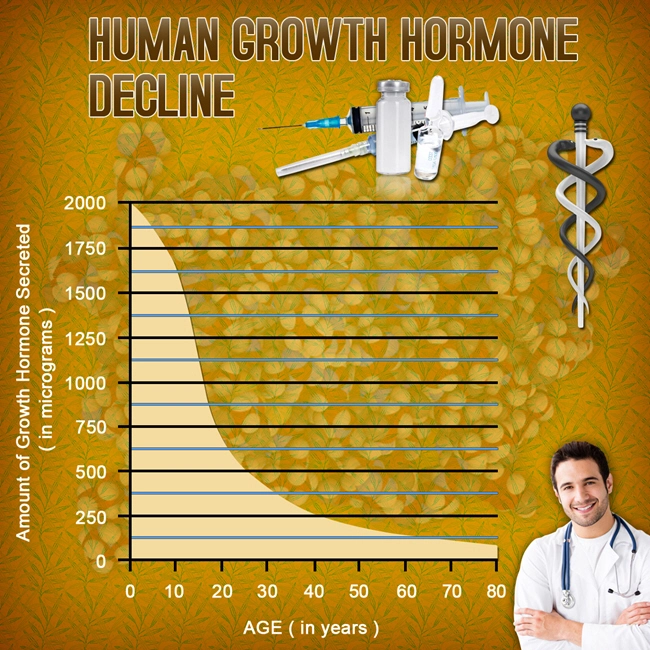
Testosterone levels decline gradually with age.
Unlike females going through menopause, the decline in testosterone in men is gradual, and there is variation among individuals.
Upon reaching 80 years of age, the rate of testosterone secretion has decreased by about 50% for men.
The American Association of Clinical Endocrinologists defines hypogonadism as a testosterone level that is below the lower limit of normal for young adult control subjects.
 Researchers conclude there is no black-and-white cutoff for "low" or "suboptimal" testosterone.
Researchers conclude there is no black-and-white cutoff for "low" or "suboptimal" testosterone.
Different symptoms show up at different testosterone thresholds: Muscle mass and strength do not decline until testosterone drops quite low (significantly below normal levels) whereas libido may dampen with relatively small decreases in the hormone.
According to Joel Finkelstein, associate director of the Bone Density Center at Massachusetts General Hospital in Boston, men's functioning is not impaired solely by a loss of testosterone, but by a loss of estrogen as well.
Agreement on the threshold of testosterone values below which a man would be considered hypogonadal has not been reached.
Testosterone can be measured as "free" (that is, bioavailable and unbound) or, more commonly, "total" (including the percentage that is chemically bound and unavailable).
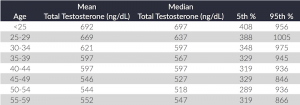 In the United States, male total testosterone levels below 300ng/dl from a morning serum sample (most accurate measurement) are considered low.
In the United States, male total testosterone levels below 300ng/dl from a morning serum sample (most accurate measurement) are considered low.
To confirm the low levels of testosterone, doctors recommend repeating the measurement of morning total testosterone.
Proponents of andropause as a distinct condition claim that it is a biological change experienced by men during midlife, and often compare it to female menopause.
Menopause, however, is a complete cessation of reproductive ability caused by the shutting down of the female reproductive system. Andropause is a decline in the male hormone testosterone.
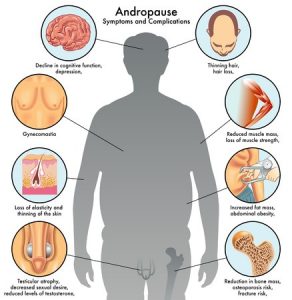
This drop in testosterone levels is considered to lead to erectile dysfunction, diabetes, loss of energy and concentration, depression, and mood swings.
While andropause does not cause a man's reproductive system to stop working altogether, many experience symptoms of impotence.
Much of the current widespread interest in the concept of andropause is fueled by the book Male Menopause, written by Jed Diamond.
According to Diamond's view, andropause is a change of life in middle-aged men, which has hormonal, physical, psychological, interpersonal, social, sexual, and spiritual aspects.
Diamond claims that this change occurs in all men, generally between the ages of 40 and 55, though it can happen as early as 35 or as late as 65.
The term "male menopause" may be a misnomer, as unlike women, men's reproductive systems do not cease to work entirely in mid-life; some men continue to father children late into their lives (at age 90 or older).
But Diamond claims that, regarding other life impacts, women and men experience similar phenomena.
The concept of andropause is perhaps more widely accepted in Australia and some parts of Europe than it is in the United States.
Many clinicians believe that andropause is not a valid concept.
Men can continue to reproduce into old age; their reproductive systems do not stop working entirely in midlife, and therefore they do not exhibit the sudden  and dramatic drops in hormone levels characteristic of women going through menopause.
and dramatic drops in hormone levels characteristic of women going through menopause.
Other clinicians have the opinion that andropause is merely synonymous with hypogonadism or unusually low testosterone levels.
There is opposition to the concept of andropause in Europe as well as the U.S.
Some clinicians argue that many of the cited symptoms are not distinct enough to warrant describing a new condition.
For example, people who are overweight may be misguided into treating a new illness rather than addressing the lifestyle that led to their being overweight.
Similarly, energy levels vary from person to person, and for individuals who are inactive, energy levels will automatically be lower overall.
While it is true that active and otherwise healthy men could, in theory, develop andropause-like symptoms, how common and widespread the phenomenon is, and whether genetics, lifestyle, environment, or a combination of factors are responsible, is currently unknown.
The significance of a decrease in testosterone levels is debated, and its treatment with replacement is controversial.
The Food and Drug Administration (FDA) stated in 2015 that neither the benefits nor the safety of testosterone had been established for low testosterone levels due to aging.
stated in 2015 that neither the benefits nor the safety of testosterone had been established for low testosterone levels due to aging.
The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attacks and stroke.
According to The American Society of Andrology in 2009, Testosterone Replacement Therapy (TRT) is recommended when both clinical symptoms and signs of androgen deficiency and verified low testosterone levels are present in aging men.
People with borderline testosterone levels may warrant a trial of testosterone according to some endocrinologists in 2003.
Testosterone supplemental therapy is sometimes recommended to improve the sense of well-being, muscle mass, strength, and bone density in men.
Adverse effects of testosterone supplementation include increased cardiovascular events (including strokes and heart attacks) and death.
The Food and Drug Administration (FDA) stated in 2015 that neither the benefits nor the safety of testosterone had been established for low testosterone levels due to aging.
 The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attack and stroke.
The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attack and stroke.
Other significant adverse effects of testosterone supplementation include acceleration of pre-existing prostate cancer growth in individuals who have undergone androgen deprivation; increased hematocrit, which can require venipuncture to treat; and, exacerbation of sleep apnea.
Adverse effects may also include minor side effects such as acne and oily skin, as well as significant hair loss and thinning of the hair, which may be prevented with 5-alpha-reductase inhibitors ordinarily used for the treatment of benign prostatic hyperplasias, such as finasteride or dutasteride.
Exogenous testosterone may also cause suppression of spermatogenesis, leading to, in some cases, infertility. It is recommended that physicians screen for prostate cancer with a digital rectal exam and prostate-specific antigen (PSA) level before starting TRT.
Before beginning hormone replacement therapy, doctors will screen for prostate cancer with a digital rectal exam and prostate-specific antigen (PSA) level and monitor PSA and hematocrit levels closely during the treatment.
The impact of low levels of testosterone has been previously reported. In 1944, Heller and Myers identified symptoms of what they labeled the "male climacteric" including loss of libido and potency, nervousness, depression, impaired memory, the inability to concentrate, fatigue, insomnia, hot flushes, and sweating.
 Heller and Myers found that their subjects had lower than usual levels of testosterone and that symptoms dramatically decreased when patients were given replacement doses of testosterone.
Heller and Myers found that their subjects had lower than usual levels of testosterone and that symptoms dramatically decreased when patients were given replacement doses of testosterone.
Andropause may also be associated with Alzheimer's disease, according to a 2007 study.
The term "symptomatic late-onset hypogonadism" (or "SLOH") is sometimes considered to refer to the same condition as the word "andropause."
Some researchers prefer the term "androgen deficiency of the aging male" ("ADAM"), to more accurately reflect the fact that the loss of testosterone production is gradual and asymptotic (in contrast to the more abrupt change associated with menopause).
References:
Andropause: The Male Menopause
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- New Research on Hormone Replacement Therapy [Last Updated On: December 29th, 2024] [Originally Added On: March 12th, 2021]
- LCN2 Hormone Suppresses Hunger and Stops Cravings! [Last Updated On: January 27th, 2025] [Originally Added On: April 7th, 2021]
- Melatonin: The Body's Master Clock [Last Updated On: December 27th, 2024] [Originally Added On: April 8th, 2021]
- The Importance of Luteinizing Hormone [Last Updated On: December 28th, 2024] [Originally Added On: April 11th, 2021]
- Finally Explained: The Mysterious Pineal Gland [Last Updated On: December 28th, 2024] [Originally Added On: April 30th, 2021]
- Hormone Therapy May Help Cut Alzheimer's Risk [Last Updated On: November 24th, 2024] [Originally Added On: May 18th, 2021]
- Androgel : Men Getting Their Mojo Back! [Last Updated On: May 12th, 2025] [Originally Added On: May 21st, 2021]
- HGH Secretagogue [Last Updated On: November 24th, 2024] [Originally Added On: May 22nd, 2021]
- Hormone Replacement Therapy Safe, Study Suggests [Last Updated On: May 17th, 2025] [Originally Added On: May 24th, 2021]
- The HGH Recommended Medical Dosage - The Importance of Blood Work [Last Updated On: November 24th, 2024] [Originally Added On: May 25th, 2021]
- Act Now to Prevent the Increasingly Common Condition of Hypothyroidism [Last Updated On: October 23rd, 2025] [Originally Added On: June 21st, 2021]
- A Toxic Hormone is Altering the Sex and Reproduction of Aquatic Life in United States Streams [Last Updated On: November 24th, 2024] [Originally Added On: August 16th, 2021]
- New Research: Cognitive Therapy Could Reduce Menopausal Hot Flashes [Last Updated On: November 23rd, 2024] [Originally Added On: August 16th, 2021]
- Heart Benefits From Hormone Replacement Therapy? [Last Updated On: November 22nd, 2024] [Originally Added On: August 18th, 2021]
- Risks of Hormones in Early Menopause Challenged [Last Updated On: November 21st, 2024] [Originally Added On: August 24th, 2021]
- Comprehensive Hormone Replacement Therapy with Tesamorelin [Last Updated On: May 5th, 2025] [Originally Added On: September 18th, 2021]
- Early Hormone Replacement Therapy May Lower Alzheimer Risk [Last Updated On: November 14th, 2024] [Originally Added On: October 25th, 2021]
- Stimulate HGH: Growth Hormone Secretagogue: Sermorelin Acetate [Last Updated On: November 20th, 2024] [Originally Added On: October 25th, 2021]
- Growth Hormone Therapy Reverses Biological Age In Groundbreaking Study [Last Updated On: November 11th, 2024] [Originally Added On: October 25th, 2021]
- Estrogen HRT May Reduce Breast Cancer Risk [Last Updated On: November 9th, 2024] [Originally Added On: October 26th, 2021]
- Hormone Replacement Therapy is Safe [Last Updated On: November 15th, 2024] [Originally Added On: October 26th, 2021]
- The Benefits of IGF-1 [Last Updated On: November 10th, 2024] [Originally Added On: October 26th, 2021]
- Insulin-Similar Growth Factor Benefits [Last Updated On: November 16th, 2024] [Originally Added On: October 26th, 2021]
- Growth Hormone Dosage [Last Updated On: November 8th, 2024] [Originally Added On: October 26th, 2021]
- Growth Hormone Sprays [Last Updated On: November 7th, 2024] [Originally Added On: October 26th, 2021]
- The Best Ways to Boost Growth Hormone [Last Updated On: November 13th, 2024] [Originally Added On: October 26th, 2021]
- Growth Hormone Explained [Last Updated On: November 17th, 2024] [Originally Added On: October 26th, 2021]
- What Men Need To Know About Testosterone And Growth Hormone [Last Updated On: November 5th, 2024] [Originally Added On: October 26th, 2021]
- Growth Hormone and Gene Therapy [Last Updated On: November 6th, 2024] [Originally Added On: October 26th, 2021]
- Growth Hormone and the Law [Last Updated On: November 4th, 2024] [Originally Added On: October 27th, 2021]
- Growth Hormone and the Hypothalamus Gland [Last Updated On: November 3rd, 2024] [Originally Added On: October 27th, 2021]
- Growth Hormone and Testosterone Replacement Therapy [Last Updated On: January 2nd, 2025] [Originally Added On: October 27th, 2021]
- Growth Hormone and Pneumonia [Last Updated On: November 2nd, 2024] [Originally Added On: October 27th, 2021]
- An Introduction to Growth Hormone [Last Updated On: November 1st, 2024] [Originally Added On: October 27th, 2021]
- General Physician Versus Hormone Specialist – Some Symptoms Require a Specialist to Heal [Last Updated On: September 6th, 2025] [Originally Added On: March 18th, 2022]
- Hormone Impacts And Function Of HGH [Last Updated On: December 20th, 2024] [Originally Added On: July 10th, 2022]
- Cheaping Out on HGH Therapy – JUST DON’T DO IT [Last Updated On: September 18th, 2025] [Originally Added On: July 12th, 2022]
- Slow Aging with Growth Hormone [Last Updated On: May 27th, 2025] [Originally Added On: July 17th, 2022]
- Hormone Therapies: How They Have Evolved and Are Evolving [Last Updated On: September 10th, 2025] [Originally Added On: February 10th, 2023]