Video Link: https://vimeo.com/286855648
Video Download: Osteoporosis What It Is And How You Can Fight And Avoid It Part 1
Video Stream: Osteoporosis What It Is And How You Can Fight And Avoid It Part 1
Video Link: https://vimeo.com/286855936
Video Download: Osteoporosis What It Is And How You Can Fight And Avoid It Part 2
Video Stream: Osteoporosis What It Is And How You Can Fight And Avoid It Part 2
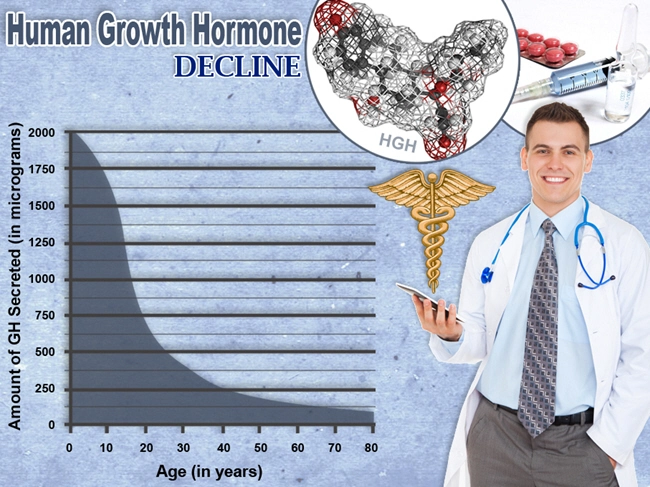
The benefits of Human Growth Hormone (HGH) Replacement Therapy are well-known: skyrocketing energy, better sleep, stress control, more enthusiasm, stronger muscles, and more.
But a lesser-known benefit of growth hormone restoration is increased bone strength. Our specialty is hormone replacement, but our mission is to provide advice in all aspects of regaining and maintaining your continued good health, and that includes facing the hideous reality of osteoporosis and what you can do about it.
In spite of protestations to the contrary, aging is a disease...period. Nothing, absolutely nothing about our bodies improves over time.
And our bones are subject to the damage that aging inflicts on any other body part. As you age, the greater your risk of osteoporosis. 
Women's bones are thinner than men's, and bone density rapidly declines after menopause.
Therefore, it's no shock that around 80% of Americans with osteoporosis are women.
But men can be stricken with this affliction as well. Granted, osteoporosis is much more common in women, but men are at risk, too.
In fact, about 25% of men over 50 will have an osteoporosis-related fracture. Osteoporosis may be under-diagnosed in men because it is often considered a "woman's disease" and men may not be tested.
When considering what you can do to prevent osteoporosis, you first need to be aware of what causes it, and why some people develop it and some don't.
There are specific risk factors beyond your control:
- Thin, small-framed women have a greater chance of developing osteoporosis.
- Genetics. If osteoporosis runs in your family, the odds are higher than it may strike you as well
- Ethnicity. Whites and Asians suffer osteoporosis more frequently, but African-Americans and Hispanics may also be at risk
- Other health conditions. Type 1 diabetes, rheumatoid arthritis, inflammatory bowel disease, and hormonal disorders are also related to bone loss.
The Good News? There Are Risk Factors You Can Control
Several debilitating lifestyle choices elevate your risk of osteoporosis: smoking, excessive alcohol intake, not exercising, and poor eating habits are also connected to bone loss and a chance of fractures.
Also, anti-inflammatory drugs that are used to treat asthma and other conditions, and eating disorders (anorexia nervosa or bulimia) also boost your risk of bone loss.
How Do You Know if You are Developing Osteoporosis?
Your physician may order a bone mineral density test if:
- You're older than 50 and have fractured a bone
- You're are a woman past 65 or a man past 70
- You are in menopause or p0st menopause and have other risk factors
- You are a man between 50-69 with risk factors
DXA (dual X-ray absorptiometry) is a brief 15-minute test that uses low-dose X-rays to measure bone density.
How to interpret Your T-score
The test contrasts your bone mineral density (BMD) with that of a healthy 30-year-old. This is the age that bone mass is at the strongest and thickest. The results come as a T-score in these ranges:
T-score in these ranges:
- -1.0 and higher is normal bone density
- Between -1.0 and -2.5 shows low bone density (osteopenia) but not osteoporosis
- -2.5 or lower indicates osteoporosis
- As your bone density drops, so does your T-score
Treatment: Bone-Strengthening Drugs Might be beneficial, but they can also be a Double-Edged Sword
If you are diagnosed with osteoporosis, you may be prescribed one of a number of drugs called bisphosphonates: Actonel, Boniva, Fosamax, or Reclast.
They can slow bone loss and fracture risk and can help reconstruct bone density.
But they can also deliver some hellish side effects: if taken orally, they can produce gastrointestinal problems like ulcers in the esophagus, acid reflux, and nausea. Injectable bisphosphonates can cause flu-like symptoms.
Bisphosphonates may elevate the risk of jaw bone destruction. Hormone replacement therapy, once used widely for menopause symptoms, is an alternative for osteoporosis, but it's used less frequently than other medications because of cancer risk, blood clots, heart disease, and stroke.
Evista is not a hormone but can deliver comparable bone-strengthening effects to estrogen minus cancer risk like blood clots and increased hot flashes.
Forteo, a synthetic parathyroid hormone, requires daily injections and builds new bone. Leg cramps and dizziness have been reported with Forteo use.
Prolia is a lab-manufactured antibody that inhibits the break down of bone. Injected twice a year, it is designed for postmenopausal women at serious risk for fractures who can't tolerate other osteoporosis drugs or who haven't benefitted from other medications.
Side effects include back pain, muscle pain, bone pain, a greater risk of infections, and diminished calcium levels. Most medications for osteoporosis slow bone loss or slightly boost bone density.
Forteo helps build new bone, but requires daily injections and can only be used for two years because of potential side effects. But there's a glimmer of hope for a cure for osteoporosis.
New research in animals indicates that an experimental drug that blocks serotonin from being synthesized in the gut could build new bone and reverse bone loss.
How to Avoid the Drug Merry-Go-Round
There is no debating the fact that the ancient cliché: “an ounce of prevention is worth a pound of cure,” applies to osteoporosis as well.
There's no question that the drugs mentioned earlier can work wonders for some people.
But for others, the side effects may be worse than the disease.
Therefore, you owe it to yourself to try to avoid needing those drugs in the first place. Putting calcium-rich foods on your plate can help protect your bones no  matter how old you are.
matter how old you are.
Drinking the equivalent of three and a half 8-ounce glasses of vitamin D-fortified milk provides bone protection.
Fish such as salmon, tuna, and herring are loaded with vitamin D, which allows us to absorb calcium. And don't forget the magnesium found in leafy green vegetables that also helps maintain good bone quality.
Many foods and drinks such as cereals and orange juice deliver calcium and vitamin D.
Foods to Avoid That are Bad to the Bone
Some foods can crater your body's calcium, such as...
- Salty foods like canned soups and processed meats. These foods are loaded to the gills with sodium. We do need some sodium, but this need can be satisfied by eating foods in their natural state as much as possible
- A cup or two of coffee daily can deliver health benefits. But several cups may be too much of a good thing, since that amount may inhibit your body's absorption of calcium.
- Moderate drinking is fine if restricted to moderation (two drinks per day for men and one for women), but excessive alcohol consumption can result in bone loss.
Don't Forget Supplements
Most people ingest sufficient calcium, except girls ages 9-18. Two types of calcium supplements are commonly available: calcium carbonate and calcium  citrate, which produce similar beneficial results.
citrate, which produce similar beneficial results.
To improve absorption of calcium supplements, take half the dose in the morning and a half later in the day. Excess calcium can cause kidney stones, so make sure to research the upper limit for calcium.
Don't forget to keep your levels of vitamin D high since that assists the absorption of calcium.
The Crucial Role of Exercise
Strength training can help you build bone and maintain it. That includes walking, jogging, tennis, and other activities where you move your entire body weight.
Using small weights in different ways also helps bones. Women who walk a mile daily have between four to seven more years of bone reserve, according to research. But you need to be cautious and don't overdo it.
Yoga and Pilates can work wonders with balance and flexibility, and both are strongly recommended. However, excessive twisting or forward-bending can skyrocket the risk of spinal compression fractures in people who have osteoporosis.
High-impact training also can be risky for people with weakened bones. Swimming and bicycling are fabulous exercises, but they are not weight-bearing and won't provide bone-health benefits. 
Another form of exercise to help increase your balance is the stability ball. There are several different movements performed on and with the ball that can add stability to your walking, and give help in preventing falls.
Books, magazines, the Internet, and personal trainers can all offer instruction on using a stability ball. Falling is a grave concern for anyone, especially senior citizens.
Many seniors never recover from a severe fall, so the time to work on balance and flexibility is now! Avoiding fractures is also key to keeping your bones healthy, whether you have bone loss or not.
In addition to exercise, fall prevention includes minimizing clutter and ensuring that your area rugs are anchored to the floor. Toss throw rugs and loose cords. Wearing sturdy, rubber-soled shoes also can reduce the risk of falling.
Osteopenia: Borderline Bone Loss
If you are starting to experience bone loss but not enough to be osteoporosis, you might have a condition known as osteopenia. Like osteoporosis, there are no outward, noticeable symptoms. Osteopenia may progress to osteoporosis, but by eating smart and moving like recommended above, you can impede bone loss. Your doctor will determine if you need medication.
Get an Early Start to Prevent This Nightmare
Developing healthy habits early in life can pay significant dividends years down the road with powerful bones. Young people can strengthen their bones by eating calcium-rich foods, getting enough vitamin D (through sunshine or diet), and exercising regularly. Here are the recommended daily intakes of calcium by age:
- Under one year: 200-260 mg
- 1-3 years: 700 mg
- 4-8 years: 1,000 mg
- 9-18 years: 1,300 mg
- 19-50 years : 1,000 mg
- 51-70 men: 1,000 mg
- 51+ women: 1,200 mg
- 71+ years: 1,200 mg
By age 30, the average woman has built 98% of her peak bone mass.
More Good News: It's Never Too Late to Build Bone Health
Most folks don't know about their bone loss until they are in their 60s or older. But even then you can still reverse the trend by increasing calcium intake to  recommended levels and exercising regularly.
recommended levels and exercising regularly.
And never forget this: osteoporosis does not have to control your life. Being a couch potato will make a bad situation worse and your bones will weaken further. So keep moving!
If you have balance issues, get help carrying heavy grocery bags or other items, and use railings, a cane, or a walker, but try your best to complete these things by yourself.
When combined with the ideas mentioned, growth hormone replacement is the sentinel that will provide protection from the monstrous affliction of osteoporosis. To learn more contact us for a FREE, no-obligation discussion of the miracle of growth hormone.
References
An overview and management of osteoporosis
The Epidemiology and Pathogenesis of Osteoporosis
Contact Us Today For A Free Consultation
Dear Patient,
Once you have completing the above contact form, for security purposes and confirmation, please confirm your information by calling us.
Please call now: 1-800-380-5339.
Welcoming You To Our Clinic, Professor Tom Henderson.

- Are You Constantly Feeling Tired And Fatigued ? [Last Updated On: November 25th, 2021] [Originally Added On: May 1st, 2018]
- Constantly Tired? Can't Sleep? [Last Updated On: April 10th, 2024] [Originally Added On: March 23rd, 2019]
- How to Understand and Deal with Cirrhosis [Last Updated On: April 9th, 2024] [Originally Added On: April 12th, 2019]
- Insomnia: The Silent Killer [Last Updated On: April 8th, 2024] [Originally Added On: April 30th, 2019]
- Lipocine Reintroduces Tlando [Last Updated On: April 16th, 2023] [Originally Added On: March 18th, 2020]
- High-Intensity Interval Training Boosts Both Body and Mind [Last Updated On: March 24th, 2024] [Originally Added On: May 10th, 2020]
- Tattoo Safety: What to Know Before You Get a Tattoo [Last Updated On: April 1st, 2024] [Originally Added On: June 2nd, 2020]
- Testosterone and Fatherhood [Last Updated On: November 25th, 2021] [Originally Added On: October 12th, 2020]
- L-Arginine: The Key to Both Heart Health and Sexual Health [Last Updated On: April 6th, 2024] [Originally Added On: December 4th, 2020]
- The Importance of Hormonal Balance for Menopause [Last Updated On: March 25th, 2024] [Originally Added On: December 14th, 2020]
- Menopause Drugs: Study Stokes New Debate Over Cancer Risks [Last Updated On: April 4th, 2024] [Originally Added On: December 16th, 2020]
- Study Examines Link Between Growth Hormones and Osteoporosis [Last Updated On: April 7th, 2024] [Originally Added On: December 17th, 2020]
- Everything You Need to Know About Clomiphene [Last Updated On: April 5th, 2024] [Originally Added On: December 20th, 2020]
- Fast Facts About DHEA: What You Need to Know About This Natural Steroid [Last Updated On: April 15th, 2023] [Originally Added On: March 4th, 2021]
- Enjoy a Few Drinks Weekly? Beware: This May Be a Link to Low Sperm Counts and Quality [Last Updated On: April 2nd, 2024] [Originally Added On: August 16th, 2021]
- Hormone Therapy May Benefit Some Women's Hearts [Last Updated On: March 23rd, 2024] [Originally Added On: August 18th, 2021]
- HGH Male Blood Panel [Last Updated On: October 28th, 2021] [Originally Added On: September 28th, 2021]
- Growth hormone = More Sleep = Better Sex! [Last Updated On: April 3rd, 2024] [Originally Added On: October 11th, 2021]
- Low Testosterone and Hypogonadism: The Difference [Last Updated On: March 16th, 2022] [Originally Added On: October 12th, 2021]
- The Link Between Testosterone and Tylenol [Last Updated On: March 26th, 2024] [Originally Added On: October 12th, 2021]
- Hormone Replacement Therapy and Aerobics May Ease Menopause Symptoms [Last Updated On: March 22nd, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone and Lifestyle = An Extended Lifespan [Last Updated On: March 28th, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone, Foods, and Supplements for Healthy Skin [Last Updated On: March 15th, 2022] [Originally Added On: October 13th, 2021]
- Hormone Replacement Therapy, Menopause, and Cancer [Last Updated On: March 29th, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone, Exercise, and Osteoporosis: The Facts! [Last Updated On: March 27th, 2024] [Originally Added On: October 13th, 2021]
- Hormone Replacement Therapy and Menopause [Last Updated On: March 30th, 2024] [Originally Added On: October 13th, 2021]
- Testosterone and Women [Last Updated On: March 20th, 2024] [Originally Added On: October 13th, 2021]
- Growth Hormone and Smoking [Last Updated On: March 21st, 2024] [Originally Added On: October 14th, 2021]
- Testosterone, Statins, and Prostate Cancer [Last Updated On: March 19th, 2024] [Originally Added On: October 19th, 2021]
- Researchers Investigate Declining Sperm Counts, Find Chemicals Rampant [Last Updated On: June 24th, 2022] [Originally Added On: June 14th, 2022]